More Stories from Our Community
Read more stories about communities coming together during the COVID-19 pandemic.
Sharing Critical Information

©Bill & Melinda Gates Foundation/Charina Pitzel
“Accessibility is not just a checklist. It’s a philosophy.”
Elizabeth Ralston (she/her), Independent Accessibility Consultant
I’m always thinking about things from a health and equity perspective. My work is at the intersection of community health, nonprofits, and accessibility. As a consultant, I primarily help organizations with capacity building by helping them engage more people in an accessible way. I’m also the founder of the Seattle Cultural Accessibility Consortium, which helps arts organizations improve accessibility for people of all abilities.
The term “accessibility” means being able to easily use something. It could mean being able to physically enter a place or it could mean access to knowledge. The need for this work is critical because, if there are barriers to access, then a person won’t have equal opportunities as everybody else.
I have lived experience with hearing loss and I have two cochlear implants to help me hear. So, while I don’t understand all disabilities, I have developed a good understanding of what people with different circumstances may need in order to access information.
Emergency access
When the pandemic started, I thought, “How can I help disability communities access information about COVID?” I reached out to the King County Department of Public Health, where I used to work, and encouraged them to make their communications more accessible.
For people with low- to no vision or hearing, we created videos. I filmed a video with a colleague who signs, where we talked about our different strategies in coping with being unable to read lips while people are wearing masks. We used captions and audio description in the video. We also created videos and messaging for neurodivergent people and people with cognitive disabilities, because there are a variety of ways that people can interpret information, depending on how their brains work. For people in the deafblind community who communicate with tactile interpreters (the deafblind person feels the interpreter signing into their hands), it’s been especially challenging as tactile interpretation is very difficult to do when you’re six feet apart. To address this challenge, we developed pamphlets in large print and in braille.
Vaccination was an important part of this communication effort. One of our working groups launched a special vaccine clinic for people with disabilities. We used targeted campaigns to communicate that vaccines were available in the first place, because people with hearing loss won’t be able to just overhear that information on the radio. We helped people access information about where to get vaccinated, but we also organized transportation, as that can be a big barrier for people with physical disabilities or who are blind or have low vision.
It was also important to educate the staff at the clinic about making various considerations for a variety of disabilities – not only people with sensory issues, but also invisible disabilities that can include mental health issues, such as post-traumatic stress disorder, autism, or anyone who is neurodivergent.
Making universal access the starting point
The pandemic unearthed a lot of inequities, particularly in BIPOC communities. It’s highlighted for me that intersectionality is a big issue because the more layers you pack on top of any single barrier, the harder it is for people to access anything – arts, education, healthcare. You have to consider the immigrant whose second language is English. How are they going to access this information?
As all of us age, we get more and more disabilities, whether they’re temporary or permanent. In the next 10 years, we’re going to get an explosion of an elderly community, and we have to think about how these people can access their own healthcare. It costs taxpayers more money if we don’t include people with disabilities in policy setting, in education, in healthcare, in any kind of planning.
Accessibility doesn’t have to cost that much, especially if you plan from the very beginning using a universal design perspective and build relationships with disability communities in the advocacy and hiring process. Accessibility is not just a checklist. It’s a philosophy that must be integrated within the organization. And if that’s not enough motivation, people with disabilities represent a billion-dollar industry. If we’re represented, we will show up.
Inclusion as a means to equitable access
What makes me hopeful is that people are starting to listen more and realize that they need to do better. The pandemic has helped make my work more accessible because it’s mostly virtual. Video calls are a perfect example of how easy it is for anybody to take a meeting or turn on captions. Theaters are more likely now to provide services like captioning upon request, so someone like me doesn’t have to plan their month around a single performance. I still have to call ahead, and my friend has to call ahead and make sure there’s wheelchair access, but someday I hope we can be spontaneous and just step off the street and buy a ticket to a show.
I think a lot of people are uncomfortable with the idea of accessibility because they don’t know how or where to start. They have preconceived notions about what people with disabilities want and need. So, the first step is to become really familiar with your audience. Include us in those conversations. As we do diversity, equity, and inclusion work, the accessibility piece needs to be part of that – so we’re working to dismantle ableism alongside dismantling racism.
To be any kind of ally, the best thing you can do is to be open, curious, and brave enough to lean into your discomfort. And when you hear or see something that doesn’t seem right with you, speak up.
– Told to Thanh Tan, independent journalist, January 2022
Website | elizabethralston.com

©Bill & Melinda Gates Foundation/Alex Garland
“Whether it’s issues around mass incarceration, deportation, or houselessness, it impacts my friends and family.”
Oloth Insyxiengmay (he/him), Asian Pacific Islander Cultural Awareness Group (APICAG)
I’m an organizer. I do work around prisoner support, prisoner advocacy, prison abolition, and anti-deportation. I also work with a lot of collectives. Whether it’s Freedom Project WA, Asian Pacific Islander Cultural Awareness Group (APICAG), the Rooted ReEntry Collective, Free Them All WA, or others, the work is usually around the criminal legal system or carceral systems, where the folks who are disproportionately impacted are – unfortunately – Black, Indigenous, folks of color, and Southeast Asian folks.
It’s work I can’t escape, since family members, friends, and people in proximity with me are impacted by these systems every day. That’s the community I’m from.
Lockdown in Lockup
In the pandemic, a lot of us forget that there are incarcerated and detained communities, not just individuals but also families who are caged – and that they’re dealing with COVID-19 too. People who have never dealt with the carceral system don’t know it was already a struggle to get the departments of corrections to give appropriate treatment for any medical problem.
COVID has compounded that. There’s not a lot of space in these places, by design, so it’s nearly impossible to social distance. If there’s an outbreak, a lot of times they put sick folks into an even smaller area or throw them in the hole (solitary confinement), which effectively punishes them for having COVID. This comes on top of the concern that folks won’t get proper medical treatment if they get COVID.
We do a lot of work around advocating for medical treatment, advocating for someone’s release, or talking to policymakers. Our focus is on holding the DOC, policymakers in Olympia, and other people in power accountable for caring for our folks. We push for laws and policies that not only get people out, but also provide resources both before and after their release, so they not only survive but also thrive on the outside.
Building care, transforming justice
When Governor Inslee passed the initiative to release folks due to the pandemic, we started to build a community collective to support folks coming home. Many folks don’t realize that reentry work intersects with fighting houselessness. When folks come out, if they don’t have the support they need, they can fall into homelessness … and when they’re in poverty, they’re more likely to be reincarcerated.
People have the idea that criminal behavior is the responsibility or the fault of the incarcerated person, so they don’t think that person deserves help. But, in fact, systems of inequity and marginalization trap folks into situations that get them into the legal system in the first place … and once they’re stuck in that system, there are often no resources to get out.
Our work tries to help people see that it’s the responsibility of the system that caused that situation to help people get out of it.
My family was displaced from Southeast Asia due to U.S. aggression and U.S. policy in Southeast Asia. We came as refugees to a country we didn’t know and got placed in poor, under-resourced communities. When I was younger, I was excited about school, but I ended up falling into some of the stuff that comes with poverty. I was incarcerated at 15 years old, but I began to make connections with community members inside, like folks in APICAG. They provided the resources I needed: love and care and space to read, write, reflect, learn, and think about what it means to be someone like me in this society.
It’s not a coincidence that the faces I saw in my neighborhood were the same faces sitting across from me in prison. I can’t talk to a family member or a friend without that family member or friend being proximate to somebody who is being sentenced or currently detained or facing a judge.
Whether it’s mass incarceration, deportation, or houselessness, it happens because of racism and because of all the things that put the wealthy and privileged in one space and poor people of color into a marginalized space.
It’s a heavy feeling, and the pandemic just made it harder to navigate these systems. Usually, we navigate them together through relationships, but relationships have become more difficult during this time. I think it has a lot to do with unaddressed trauma that our communities disproportionately deal with, and therapy isn’t readily accessible for a lot of us. There’s no way to turn that off and “relax” or “reground” or “find ourselves” in this pandemic.
All we can do is organize, organize, organize.
Re-evaluating resources
Folks doing this work all resonate on the same sentiment: “We don’t have enough resources for all the folks out here that need support.” As one of the richest cities in the world, Seattle has resources, but what we’re doing about houselessness isn’t working. Continuing to do sweeps, moving folks around to different locations, trying to put them in housing without providing culturally responsive treatment … it doesn’t change anything.
When I think about my hopes coming out of this pandemic, I hope this is something we can address.
It’s hard to show up when we don’t have the resources to show up. There aren’t enough folks with the expertise and experience to do this hard community work in the first place … and when folks are able to show up to do this work, it burns them out. Non-profit jobs within Seattle pay on average $45-$65K for an annual salary, which isn’t a living wage here. But those folks are expected to show up and save the world. It can be counterintuitive for them – folks who are themselves directly impacted by racism and capitalism on an everyday basis are expected to change the system.
Maybe we can address these issues better by realizing that, if you’re thriving because you have a certain amount of resources, then the next person might need the same amount of resources to thrive as well.
– Told to Marcus Harrison Green, South Seattle Emerald, September 2021

©Bill & Melinda Gates Foundation/Alex Garland
“I hope people, especially people in power, are focused on the community.”
Sophia Brown (she/her) |
Graduate of Cleveland High
School
Fathima Garcia (she her) |
Graduate of Cleveland High
School
Sam Cristol (they/them) |
Educator at Cleveland High
School
Sophia Brown: It all started when [our teacher] Mx. Sam Cristol pitched the idea of having a vaccination clinic as a project for seniors [at Cleveland High School]. It was just an idea at that point, and we didn’t really know how it was going to happen.
Sam Cristol: The idea of a vaccination clinic was something I heard from two different educators in a staff meeting. It came from thinking about how we could make our school into a genuine resource center for the community. Because it’s a public school, it’s also a public building. It was just a question of who was going to run with this idea.
Fathima Garcia:
When Mx. Cristol brought this up, I
was super excited to be a part of
it.
Sam Cristol: I knew we had some
motivated students in the senior
class – like Fathima and Sophia –
who really care about service. They
were willing to run with it and make
it into a legacy that they’re
leaving behind.
Fathima Garcia: The culture of Cleveland High School is very community-driven. I have a passion for educating my community with the resources and tools that they aren’t fortunate enough to have. That’s what motivates me.
Sophia Brown: Especially during the lockdown [from COVID-19], there was a lot of time to get more in touch with my local community. I do running, so I spent a lot of that summer running around my neighborhood and getting to know it better. I got to really reflect on my place in Seattle.
Fathima Garcia: For all of us, COVID-19 was hard in different ways. I come from a very hardworking family. My parents both work two jobs, so it went from everyone being at school or at work to everyone being at home. At first, we didn’t really know what to do, but we made it work. We went on walks. It became a kind of family time we didn’t really have before.
Sam Cristol: I think the hardest thing was the way school shifted to being online. We did our best to build community and build relationships online, but it was hard. I know had a lot of amazing students pass through my class last year who I just don’t know very well. I felt fortunate I got some time in real-life to know students through the vaccine clinic project. We really wanted the clinic to be student-led, meaning students were working as non-medical staff. And they worked hard to make sure it became a culturally responsive clinic open to not just our students and families, but the South End community.
Sophia Brown: The South End of Seattle is a place that takes care of each other. The clinic was us taking care of ourselves. There was pride in being able to be the ones who was giving that gift to our own community.
Fathima Garcia: I think what drove us the most was to provide accessibility for our community.
Sophia Brown: We wanted to make sure that the people who need the vaccine could get to the vaccine. There wasn’t a bus line that went to the place where student workers got our vaccines, for instance. And a lot of our students and families use public transportation, so we wanted to make sure people could get here – and then feel safe when they were here. We also wanted to make it seem like it wasn’t a space where you had to get stabbed with a needle, but a place where you were doing your part to take care of the community. We wanted to make it a comfortable space. We even played music.
Sam Cristol: The student leadership did a great job of advocating for access. They made it clear: here are the reasons we set out to do this, here are our non-negotiables. Just one example, “we will have a clinic with translation services that aren’t just somebody on a phone.”
Fathima Garcia: As a Latina, a lot of my family members didn’t get vaccinated because of the language barrier. It’s that same problem when it comes to homeownership or going to banks, and I think they may be nervous because of things that have happened in their past. But there’s more trust if you’re approached by someone from your own community. When you see your own people doing something, then you will be more likely to do it too.
Sam Cristol: You guys also did a really great job of making those things a key part of the design of the clinic.
Sophia Brown: Even just the work [of building the clinic] felt like community. It was really interesting to watch people’s minds work on all the little things that you wouldn’t consider – because they know the community differently than you do. We had people who would mention certain languages we might want translators for. We had people who would bring up ideas for how to make accessibility better.
Sam Cristol: What that really makes me think of is how important relationships are to any type of social change.
Sophia Brown: It’s true. It’s the really tiny interactions with people that end up being a lot deeper than you think they would be.
Sam Cristol: We see it when a political candidate is running and they have all these lofty goals, but they don’t have any connection to the people that they’re going to represent. But you all set up this clinic, you staffed this clinic, then you interacted with folks at the clinic. There are relationships being built, and that’s a place to invest in and to continue to build.
Sophia Brown: It makes me think of a lesson we had in school about individualism versus collectivism. When you take an action, think about how it’s going to affect the others around you rather than just what the results of that action might do for you. I’m going to wear a mask not because I need to, but because it helps someone else. And it works the other way around too: give yourself the support you need. Reaching out, even if you feel very isolated, is always something you should try and do, especially during times like these.
Sam Cristol: Speaking personally, I’m just inspired to see how I can use the power and resources I am proximal to by being an educator to facilitate more students implementing the projects that they want to see and the leadership that they’re trying to do.
Fathima Garcia: A year from now, I hope people, especially people in power, are focused on the community. I hope we’re all focused not just on what you’re doing individually and what you might gain from what you do, but what we all could gain from it – together.
– Told to Marcus Harrison Green, South Seattle Emerald, August 2021
Website | clevelandhs.seattleschools.org

©Bill & Melinda Gates Foundation/Alex Garland
“People in power, people who have resources and are making the decisions, they have to step up and do something.”
Paula Houston (she/her) | Chief Equity Officer for UW Medicine in the Office of Healthcare Equity
In the Office of Healthcare Equity, our work before the pandemic was focused on making sure UW Medicine reaches the right people at the right time and in the right way, given that there are racist structures in place that disadvantage people of color and create health disparities – particularly for Black people.
Early on, it became clear to me and my team that COVID-19 would spotlight inequities in our healthcare system. One of our hospitals, Harborview, began collecting data on who was coming in for testing and what the positivity rates were by race, ethnicity, language, and housing status. Pretty quickly, we were able to see that our Black and Brown patients were experiencing stark disproportionality in infections and hospitalizations, specifically those who are Spanish-speaking and those who live in south Seattle, south King County.
Through COVID-19 response emergency funds, we opened our first testing site at Rainier Beach. Initially, people weren’t familiar with UW Medicine, but because I live in Rainier Beach and a colleague is also a south Seattle resident, we were able to leverage relationships built over the last 25 years. We met with 17 different community groups to explain why we were bringing COVID-19 testing to the community. We also saw some big disproportionality in Asian Pacific Islander communities, so we worked with the community health board that represents that community to set up some testing sites.
When it came time to shift our focus from testing to vaccines, we knew community education would be important. What we did not realize immediately was that we would need to begin that community education with our own workforce, particularly frontline workers with limited English proficiency. We wanted to ensure that they had the best information to make a decision right for themselves about getting the vaccine and, by extension, help their families and community also be accepting of getting the vaccine. So, we worked with clinician providers and interpreters who spoke 16 languages to create informational videos we called “Community Conversations- Straight Talk on Vaccines”. We encouraged staff to invite family and friends to participate and posted them on our YouTube site for anyone who wanted to use them.
Now, we do mobile vaccines and pop-up clinics all over King County, with a particular focus on South Seattle and South King County. This summer, we had a presence at the Juneteenth event held at Jimmy Hendrix Park in partnership with the Tubman Center for Health. They called it their Blaxinnation event. It was really informative to hear firsthand what some of the hesitation about vaccines is among the community. It helps to know how to give them all the information they need, instead of making them feel coerced. Our messaging is to say, “Vaccines are what’s going to help us get out of this pandemic. And until we are, you’ll want to protect yourself, your family, your friends, and your community.”
It’s intense, heavy work. Where I find my mental health therapy and where I get my emotional and spiritual reward, quite honestly, is in powerlifting. When I’m at the gym, I leave everything behind. When gyms closed due to the pandemic, many of us started makeshift workouts in our homes. A small group of us who are masters-level lifters and mostly over 50 were talking, and one teammate said, “What if we could borrow some weights from the gym and just set up our gym in my backyard?” And that’s what we did. At the time, everyone I saw was on Zoom, but I would see my gym community in-person to lift. It was time I really held sacred – and most of us hit several personal lifting records during the pandemic.
I continue to work in healthcare equity because I am beginning to see progress in reducing health disparities as we begin to dismantle white supremacist systems in our institutions that perpetuate inequities. We’re doing that by providing education and showing the data that has previously not been collected or collected and ignored. I want to be able to change the narrative about healthcare inequity and health disparities, to show that they are real. And I want to have the narrative backed up by evidence, to motivate people into action for change.
– Told to Marcus Harrison Green, South Seattle Emerald, July 2021

Yubi © Bill & Melinda Gates Foundation/Chloe Collyer
“Young people are the now.”
Yubi Mamiya (she/her) | Junior at Shorewood High School, Director of Community Outreach at Washington State Legislative Youth Advisory Council, Founder of neXt Education App, and Youth Ambassador at the Bill and Melinda Gates Foundation Discovery Center
This pandemic, as well as my work on the Washington State Legislative Youth Advisory Council (LYAC), has shown me just how powerful young people are. I’ve heard countless speakers and legislators say, “Young people are the future.” But I think that young people are the NOW. We can make change right now.
My whole goal as the Director of Community Outreach at LYAC is to advocate for youth-driven, change-making advocacy and civic engagement, because I want to give all young people equitable opportunities for the future. This starts young. It starts in our education system, just as it did for me.
In my role, I lobby for and testify on pieces of legislation that give young people, in particular marginalized students, a solid basis in real resources – whether that’s funding, technology devices, or inclusive curriculum – so as a society we’re able to deliver on an equitable education. With my nonprofit, the free neXt Education App, I focus on making learning opportunities accessible to marginalized students who may not have that now – by putting it online and making it personalized.
I hope that other young people will see and know that their voice is powerful, and that no one is going to hear it until they start sharing it.
– Told to Marcus Harrison Green, South Seattle Emerald, February 2021
Website |
Next Education App
&
Washington State Legislative
Youth Advisory Council
Facebook |
@washingtonlyac
Instagram | @yubimamiya,
@washingtonlyac, and
@nexteducationapp
Essential Workers Meeting Everyday
Needs

©Bill & Melinda Gates Foundation/Charina Pitzel
“We’ve survived pandemics before. We know how to survive.”
Shawn Thurman (he/him),
Registered Nurse, Seattle
Indian Health Board
I come from the Sac and Fox Nation
of Oklahoma, the Southern Cheyenne
Nation, the Shawnee Nation, and the
Caddo Nation – all in Oklahoma. As a
Plains Native living in the Pacific
Northwest, it’s a whole new
culture here that I’m learning
and experiencing.
For the past three years, I’ve worked as a nurse at the Seattle Indian Health Board, working specifically with the homeless Native community. People become homeless for a variety of reasons, but mostly their plans just didn’t work out and they fell on hard times. Any of us could end up in a similar situation – and when you’re there, it can be hard to navigate resources like health care.
The Seattle Indian Health Board is a federally qualified health center (FQHC) that is based in Seattle. We primarily serve the Native community, but we’ll serve anybody who walks through our doors for whatever they need – from housing to domestic violence support, to behavioral health, dental, and medical care. It’s pretty much a one-stop shop for anybody in the community.
I knew I wanted to work in the medical field after spending a lot of time in hospitals as a kid – many members of my family had health issues. So I started my collegiate career planning to become a doctor … but after volunteering in hospitals, I decided nursing is what I’m meant to do. I love every minute I’ve had in this job.
Here, we refer to people as “relatives” as opposed to “patients.” We want them to feel that connection to us as fellow Natives – so when they walk in, they feel like family and not just a number. Because of how vast our family ties stretch, Native people are not just centered on parents, siblings, grandparents, uncles, and aunts. Our way of seeing family stretches beyond those connections. Even for people outside the Native community, when they come in, they’re our relatives.
Good medicine in hard
times
When we first got reports of a new
virus, it was a mad scramble to read
up on research and track down daily
updates on how quickly COVID was
spreading and moving across the
world. This has been a
once-in-a-lifetime thing – something
we haven’t experienced since the
Spanish flu. And when you work in
health care, you know you’re
going to be on the front lines
whether you’re ready or not.
Through it all, the Seattle Indian Health Board has been innovative. We’re rising as a leader within federally qualified heath care. When our leadership, Esther Lucero and her team, requested personal protective equipment (PPE) and instead got a shipment of body bags, that was very symbolic of the federal government’s priorities. So leadership said, “We’re going to do this our way.”
That meant being flexible and intentionally listening to the people who had boots on the ground in the community. They realized we needed to bring relatives into our clinic to provide testing and vaccines and reach out to those without the means to travel to our clinic because of distance or money.
Our model uses traditional Indian medicine at its core. We have traditional medicine apprentices who come around twice a day to smudge the whole building. Our approach is also reflected in just talking to people as people – not necessarily about the vaccine, but just to get to know them. We use humor, which is almost universal in the Native community. Humor is always good medicine. When someone knows and trusts you, they’re more likely to come around. If they don’t, then you continue to love them and treat them as a member of the community.
Bringing that good medicine in everything we do has helped us build a model that translates to other FQHCs in other cities too. Through this model, we ended up securing more than enough PPE, we were the first organization within Washington State to get the Moderna vaccine, and our vaccination rates from the beginning far exceeded state levels. We made it our mission to continue to go to those people who didn’t take the vaccine on the first try. For some, it took two, three, four visits to convince them that the vaccine was safe. It’s a long game. You have to be patient.
Trauma-informed care
As the pandemic went on, it hit me
pretty hard. A lot of people have
left health care, and I understand
why you would. The burnout is real.
It wears on you to keep seeing
relatives coming in sick. But seeing
the relatives I know, those with
whom I’ve really connected,
that’s my driving force.
COVID magnified and amplified inequities in our communities. The homeless population got fewer resources than anyone, and there was a lot of fear coming from misinformation. That really motivated me to push for Native providers and for testing – and to reframe how to talk with people. You can’t say “stay home,” if you don’t have a home to go to. If it looks like we don’t understand something so basic, someone might think, “Oh, they’re not going to help me,” and fail to seek treatment or vaccination.
Equity issues and distrust aren’t new problems. They have lasted generations since the federal government first started interacting with Natives. A lot of historical trauma plays a huge part in how sick people are getting within our community. That history includes forced sterilizations and shipping people off from their homelands to big cities all across the country without resources. That trauma has carried through generations. Even our diet as Native people is not our original diet, and we now have a lot of diabetes and heart disease in the Native community. If you get COVID with those conditions, you’re already going to get hit a lot harder. It’s so complex, and there are so many factors that are contributing to how COVID is hitting the Native community.
When people look at Native culture, they often look at us as if we’re a relic of the past. When they step into our clinic, they’re like, “Oh my gosh, you guys are … still here.” We’ve survived pandemics before, and we’re going to push through this one too. We know how to survive. It can happen if we get back to traditional ways of taking care of each other.
Keep an open mind about the people around you. Think about the larger community among the people you interact with. It’s not just about “self.”
– Told to Thanh Tan, independent journalist, December 2021
Website | sihb.org

©Bill & Melinda Gates Foundation/Charina Pitzel
“Early care and education is part of this country’s infrastructure.”
Lois Martin (she/her), Director, Community Day Center for Children
I was born and raised in Seattle’s Central District, where I own and operate the Community Day Center for Children. My mother, Lula Martin, founded the center in 1963 as a safe haven for single mothers. She and my father, Loy Martin, were foster parents and saw a community need for extra family assistance. Back then, the center had three or four children. Now, we have 40 children, ages 1 to 5, and 15 staff, including myself.
It wasn’t my plan to work in this field. From an early age, I was determined to become a “Black YUPPIE,” or “BUPPIE.” I studied computer science and accounting and worked for IBM. While on maternity leave, I began helping my mother with the center’s books. IBM offered a buyout to employees and I elected to leave, to work in the early care and education field. I now have a Master’s in Human Development and a Certificate in Early Care and Education Leadership from Harvard’s Graduate School of Education.
My introduction to the field began in the classroom as an aide. By the time my mother retired, I had enough experience to become the center director. I am intentional in my efforts to provide a wonderful early learning environment for children. When people use the term “daycare,” I gently correct them. Our teachers aren’t babysitters; they’re educated professionals with expertise in early care and education.
Essential but unsupported
In December 2019, when COVID was first discovered in Wuhan, I knew a pandemic would soon hit the West Coast. I reached out to the Department of Children, Youth, and Families (DCYF), only to discover there was no plan in place to prepare for what would soon be a crisis.
After Seattle had the first U.S. fatality in late February 2020, our center closed for a month. As things opened up, those of us in early care and education were considered essential frontline workers. Some parents stayed home with their children to wait it out, but others didn’t have that option – and we needed to be there for them. So, in April, the center reopened with just seven children.
I didn’t know how we were going to make ends meet. We wanted to keep our staff working and paid. The majority of our staff are women of color, quite a few of us are over 50, and some have diabetes or high blood pressure. We opted to give our teachers hazard pay using small grants from various organizations. These monies helped us keep our doors open. Over the summer, parents slowly began to come back … but by September, our reserves were pretty much gone.
We were so utterly on our own. Even now, two years later, speaking about this is still extremely difficult and emotionally raw.
I had to design our protocols myself, based on CDC guidelines – there simply was no support at the beginning of the pandemic. Locating personal protective equipment (PPE) or supplies was challenging. But, with the center’s community of parents, teachers, and the early care and education community at large, we began to figure it out. We came together and supported each other. Parents or directors would message when PPE was found. “Costco has paper towels.” “Lowe’s has bleach.” We worked hard to assure a safe, healthy environment for our children – and we haven’t had one case of COVID in our center.
Our ability to survive comes down to how resilient early care and education teachers and directors can be. In the early care and education community, Susan Brown at Kids Company pulled together the Greater Seattle Child Care Business Coalition (GSCCSB). This group of center directors and owners have supported each other through this pandemic with shared protocols, exchange of resources, and doing whatever we needed to keep our doors open.
The payroll protection grant was a blessing. We wouldn’t be open now if it wasn’t for federal assistance during this ongoing pandemic. I am hopeful more funds will be forthcoming, directed to our industry.
Childcare as a public good
From the beginning, it was understood that public school teachers would teach from home – but that courtesy was never extended to early care and education. People view educators who work with little children differently.
In time, we will see how a lack of childcare will impact society. If you move children out of structured environments, it can influence their ability to meet educational milestones, even years later – this is especially true for marginalized families. How do we make up that lapse in time, and will we ever be able to? Women have left the workforce to take care of children. Some men have, but the majority are women. What advancements will be missed if brilliant working women have to stay home? What are we losing by not having this generation of workers? How will that impact our country’s innovation?
Early care and education is part of this country’s infrastructure. It’s a public good and a societal need. We need real investment – and third-party investments – to support families with small children. It must be an economic priority in the same way we invest in public schools, roads, bridges, or food supply chains. Parents should have the ability, regardless of income, to access the best learning environment for their child.
That is my takeaway from this pandemic. We can’t just invest in preschool and pre-K. We need to invest in the entire system, beginning at birth. Early care and education professionals support working families. We are a rock for parents. We open educational doors for future generations – and we can’t continue to work at poverty wages.
But this field instills in me a sense of hope. Children have, for the most part, been able to weather this so well. I am hopeful that – if this ever happens again – this generation will understand the sacrifices that have to be made for the good of the whole. It’s not just about your rights, but the rights of society – and children understand that better than many adults.
– Told to Thanh Tan, independent journalist, November 2021
Website | cdccinc.net

Ryan © Bill & Melinda Gates Foundation/Alex Garland
“My biggest fear and concern was bringing this virus back home to my family.”
Ryan Sheaffer (he/him) | Firefighter and EMT, Kirkland Fire Department
As a Firefighter and EMT for the Kirkland Fire Department, there are many things that we train for, but there was no blueprint for a pandemic. It was in these first few weeks that I felt the biggest impact of the pandemic. Two or three days in, we had to perform CPR on a COVID-19-positive patient at the Life Care Center of Kirkland, where the outbreak first occurred and where there were a lot of COVID-19 patients and several deaths.
Over the years, in my career as a firefighter, I’ve noticed that most people have a lot of respect and gratitude towards this profession. But last year, for the first time in my life during the pandemic, I felt somewhat ostracized for being a firefighter. There was fear, anxiety, and uncertainty. A lot of that was because of the unknown. We didn’t know how easily the virus was transmitted, or if the PPE was going to protect us. My biggest fear was not necessarily about contracting the virus myself, but about bringing it back home to my family.
We knew that signing up for this career meant dealing with any manner of first response. So, even though we hadn’t planned for this pandemic, responding to it was in our wheelhouse. Somebody needed to go out there and do the job – and to everyone’s credit, we did it.
It has been a really difficult time, but my family has always been there for me. I choose to look at this as a reset – a place to grow and learn from. The reality is that we need hope. Without hope, we don’t have much else. And I hope that this puts us in a better position as individuals and as a society when we come out of this on the other :side.
– Told to Marcus Harrison Green, South Seattle Emerald, in March 2021
Website | Kirkland Fire Department

Kelvin © Bill & Melinda Gates Foundation/Alex Garland
“My job has been to safely transport my passengers to their destinations.”
Kelvin Kirkpatrick (he/him) | Bus Driver, King County Metro
As a King County Metro bus driver for 27 years, my job has been to safely transport my passengers to their destinations while monitoring situations inside and outside the coach.
Working so closely with the public, the word that comes to mind for what I experienced at the start of the pandemic is fear. I was immediately afraid for my son with autism who is susceptible to getting sick easily. Although the union stepped in to ease fears, without knowing much about COVID-19, I didn’t feel comfortable coming to work – and I couldn’t even take precautions, as masks were sold out. So, do I call in sick? Do I wait until we know more and can figure this out? Financially, I didn’t have the luxury to wait it out. I had to go into work and hope for the best.
What has stood out to me during this time is that the “public” – people who work as janitors or who work in fast food restaurants or grocery stores, people who may not have the luxury to work from home, and those who are doing everything to make ends meet and may not have enough to pay bus fare – they are very thankful we are operating. Every time an elderly passenger steps out, they go out of their way to wave or give us a thumbs up for our work. That makes me feel good.
I hope people take advantage of the vaccination process – and that we can get back on our feet and rebuild our economy. We’ve had to cut a lot of service and lay off more than a hundred drivers because we couldn’t run empty buses. I hope we can bring those drivers back because they have families and bills too. When the economy rebounds, job security is good for people like me. It’s the positive growth we need.
I hope we can work our way out over time … so we can look back at this and say, “We went through it, but we made it.”
– Told to Marcus Harrison Green, South Seattle Emerald, in March 2021
Website | King County Metro

Richard © Bill & Melinda Gates Foundation/Alex Garland
“I feel a sense of duty that drives me to be here.”
Richard Chung (he/him) |Owner, Seward Park Market
As a Korean American born in Portland, Oregon, community has always been important to me. My father has been a community member his whole life, and I’ve always looked up to him. My father raised me by himself since I was 12. He has always been there for me and pushes me in a positive way. He started the Seward Park Market, building it from the ground up. With him aging, I took up his job. The work never stops, but it also gives purpose to be so deeply connected with the community.
I feel like the pandemic brought our communities closer together. When COVID-19 hit, stores like Safeway had limited hours. Since we’re one of the only independent stores nearby, we had a lot of people coming in for bare necessities, like toilet paper or masks. It was challenging to keep up with the supply and demand, but hopefully we provided everything they needed – or at least as much as we could.
As owner and operator, my job is making sure everyone gets the necessities and resources they need, seven days a week. I also like to check in and make sure our customers are in good health. Most of them feel like family since I’m here all the time, and they come in always to support our business. I feel a sense of duty that drives me to be here.
I feel blessed to be in a job where I get to interact with people all the time – even if it’s just asking how they’re doing or how their day has been. These kinds of interactions, especially in a tough time, are one way we can do something to help one another.
I do my best to make sure everyone gets along. It can sometimes get challenging. We had a fight turn into a physical altercation because someone didn’t want to socially distance inside our store. I only see this increasing with summer around the corner and more people venturing out. But even if they’re mean to me or trying to get violent, I calm the situation down. I don’t raise my voice and I find another solution.
I hope this pandemic ends soon … but until then, I hope everybody loves and checks in with each other and does as much as they can to help one another. That’s the only way I feel we can break out of COVID-19.
– Told to Marcus Harrison Green, South Seattle Emerald, in April 2021
Facebook |
@jackschicken
Meeting the Needs of the
Community

©Bill & Melinda Gates Foundation/Alex Garland
“Our liberation is tied. When you pour into community, community will pour into you.”
Cheryl Delostrinos (she/her), co-founder of Au Collective
We also realized there was a much larger need. We realized the communities we were connected to were on the far margins of being able to receive any type of government funding. The barriers to access were many: they spoke English as a second language, or they didn’t have a Social Security number, or they didn’t qualify as an artist, or they didn’t have access to a computer to fill out a form to get funding.
A big barrier to liberation is access to knowledge around how to connect – not just for the communities that I come from and directly work with, but also access for communities that have resources and wealth. At the time, I was hearing some people ask, “Where do I donate? How do I help?” So, our small team put our brains together on how we could move money from people who have resources to people who needed to be resourced. We already had a partnership with Benevity, and we also partnered with a LinkedIn influencer, Visa, Textio, and Microsoft as well. Altogether, we raised over $50,000.
Culturally, in a lot of our communities, it’s not an easy thing to ask for help. Many of us have trauma around money that leads to a scarcity mentality. Collectively, we need to understand the history of the wealth gap. We need to understand how wealth doesn’t necessarily look like finances, and how resources don’t necessarily look like money. Sometimes, resources look like time and energy pouring into one another through genuine connections and showing up – which happens when we understand we all have a role and we realize what our role is and how to fulfill it realistically.
All summer in 2021, I was intentional about working with community partners from different areas of Seattle, from different generations, and at different points in their career – and bringing them together under the shared value of centralizing community and decentralizing white supremacy. But we also took time to connect, to experience joy together, and to build together, support each other and share resources.
Something I heard through all of these conversations was the need for space to start building, to come together and connect, and to do it safely and in a place that felt welcoming, like home.
I am a resident of South Park, which was the neighborhood most impacted by COVID-19 – from the amount of people hospitalized due to COVID, to the loss of jobs and businesses. Here, the desire of community was to occupy more spaces along the Duwamish, to clean it up and preserve the natural habitat for animal and natural life and also for people who have been nurturing the South Park community. I was in community conversations around a plot of land right on the Duwamish River with a view of downtown Seattle. I was in the right place at the right time to learn that the landowner of that space wanted to give in some way and was willing to have it become a community space. It was an opportunity to piece everything together.
Centralizing community is the only way for our communities to survive and for us to build and live in the world that we all want to live in. We’re not trying to disrupt the system by being a part of it anymore. The pandemic has given us perspective and an opportunity to start identifying where areas of support are, what is needed. I think that people are ready to build. I think people have been ready to build. We all want the same thing – to see all our communities thrive.
I think COVID-19 has shown all of us that the structure and the system … yes, is effective in some ways, but it has also failed a lot of our communities in a lot of different ways. I’ve wanted to throw in the towel every week. But what keeps me going is the idea that when you pour into community, they will pour into you.
To see people wanting to connect, work together, come up with new ideas, it’s a reminder that what we are doing is bigger than us.
– Told to Marcus Harrison Green, South Seattle Emerald, September 2021
Website | aucollectiveseattle.com

Dionna ©️ Bill & Melinda Gates Foundation/Alex Garland
“For tribal people, everybody’s related, everybody’s linked.”
Dionna Bennett (she/her), Program Director of Campbell Farm
I live in Wapato, located on the Yakama Indian reservation where I work as the program director at the Campbell Farm, a working farm and retreat center. I’ve been working here for the past 12 years in different capacities.
The farm has always been a safe haven. As a Wapato tribal member and African American, it’s a blessing to me and our community that the farm is a constant presence that has not gone away, that it continues to be a resource. It has brought food and love and care. The “give-back” is very real, and I’m passionate about it, especially for our kids and youth. I have a big passion about meeting our youth where they are and empowering them to do something great for themselves.
For tribal people, everybody’s related, everybody’s linked. We lost a lot of people from complications with COVID-19 – and from mental health issues. It’s forced me to really step up and look outside of the box to see how we can help people, how we get to people where they need us.
We’ve always served meals. Wapato is 96% at or below poverty. That’s a really huge number. At least half live in food deserts, which means that the nearest grocery store is at least 20 minutes away. Most rely on school food programs – but then the school shuts down because of the pandemic. So, we started serving meals and even just leaving meals on doorsteps. Because we follow a lot of the school district style, every component was met. Everyone got a protein, a fruit, vegetable and a starch. Within a month, no one ever received the same meal twice – and everything was prepared from scratch. It took a lot of time and a lot of love.
Soon, we decided to start serving the elders too. Because there’s such a need, we grew programming from serving children to serving this larger population. We were serving anywhere from 300 to 400 meals a day.
Our community work grew as the pandemic continued. Our society is already set up for failure for our people. It just made it that much more difficult to see and hear the judgments of outsiders being passed onto our reservation. There are all these judgements, and it makes me emotional to feel the weight of all these judgments.
In many places, domestic violence was on the rise with the lockdown and isolation. We realized that we have a lot of domestic violence, so we started to help moms who need safety plans and extra support in this pandemic – and going forward.
We also started the New Mothers’ Program to combat the high infant mortality rate that indigenous people face. We have only one hospital on the reservation, and it takes 30 or 40 minutes to get to that one hospital – so we partnered with the Pacific Northwest Medical Institute here. They offer clinical support via Zoom phone calls. We have some nurses through the Children’s Village clinic who can help answer questions. We also went out to churches and got diapers, wipes and formula donated.
When the homeless shelter closed down in Wapato, it meant that the nearest shelter was 60 miles away. There was no place for homeless people once they closed, so we started serving them too.
I figure, at some point, I will take a break from it all once things really slow down … but you don’t think about that when you’re in the midst of it. You just do it because it needs to be done. And when you’ve lived here for as long as I have, because this is a community I’ve been born and raised in, you can’t stop because you don’t want somebody to suffer.
I get hopeful watching things kind of slowly go back to normal. Watching kids graduate from high school, seeing new life – babies who were born during this pandemic time – that all gives me hope.
– Told to Marcus Harrison Green, South Seattle Emerald, June 2021
Website |
thecampbellfarm.org
Facebook |
The-Campbell-Farm-166841460707

“Despite the struggles during this time, we’re still able to rally around each other and build up the causes we believe in.”
Kyle Melendez Daigre (he/him) | Student at ArtCenter College of Design, CA, and Exhibiting Artist & Volunteer at Onyx Fine Arts
I was in school at the ArtCenter College of Design in California last year when the COVID-19 pandemic hit. I’ve been home in Seattle since June 2020. With campus closing and everything shifting online, the collaborative process of art and artistic communities – normally an integral part of my classes – has been deeply impacted.
What was also concerning to me was that the future of Gallery Onyx, a local non-profit arts collective in Pacific Place Downtown dedicated to showcasing and celebrating artists of African descent in the Pacific Northwest, was also in peril.
I feel strongly about the importance and need for art in our communities, especially art from those that have been historically underrepresented or ignored. I’ve been a part of Onyx since I was 16. As an exhibiting artist and someone who helps prepare walls and set-up and take-down art and provides input on marketing, social media and visual aesthetics, I continued to volunteer even after I started college.
For most of 2020, there was a lot of uncertainty. Pacific Place was practically empty – and many volunteers no longer felt comfortable coming in. It was very difficult to go overnight from selling art constantly and having tons of visitors, to having nothing.
As stores opened up and foot traffic in the mall started to increase, new volunteers stepped up to help. Onyx has given me the opportunity to learn, grow and press forward on the career path I’ve chosen – and I wanted that same opportunity to be given to as many artists as possible. It’s essential to help build equity in the industry.
What I learned from this experience is the importance of a strong community. Artists who bring their work in, organizations that donate and give exposure to the gallery, and people who visit and volunteer – all of these are part of why it was possible for the collective behind Gallery Onyx to push through such a difficult time.
This pandemic has flipped everything upside down and shown how important community support is for both people and businesses rooted within those communities. It’s great that despite the struggles during this time, we are still able to rally around each other and build up the causes we believe in. This pandemic won’t last forever. It’s important to be resilient and keep supporting the people who make positive impacts on our communities to benefit both the present and the future.
Website | onyxarts.org
Facebook | @onyxfineartscollective
Instagram | @onyxfineartscollective

Kyle © Debi Gerstel
“The world is a better place when we’re not satisfied by mediocrity.”
Kyle Gerstel (he/him) | Student at Islander Middle School and Founder of KMG Center
I’m a 14-year-old musical theater geek who, when not doing schoolwork, lives and breathes theatre. However, the unfortunate but necessary halting of live theater demolished most of my life outside of school, much like Éponine’s love life in Les Misérables.
This inspired me to create theatrical opportunities for teens to stay safe, creative and connected during this moment of darkness. By creating opportunities to tell stories, I’ve been able to experience more theater and give back to the community that cultivated my love for it.
During the pandemic, I founded an experimental online improv troupe called Chimprov and I’m currently directing my middle school’s first musical in over a decade. I also wrote, directed and edited a 10-person online musical comedy called “Hamleton: A Quaranteen’d Musical.” Although I truly love Shakespeare’s stories, I wanted to make them more accessible by writing a piece that addresses the same themes while translating them to a modern setting.
The idea for Hamleton began in April 2020 when I was trying to find a new longform writing project as well as an excuse to see my friends (it was and is very difficult to get teenagers on a “social Zoom call.”) Rehearsals were held over Zoom, and the final performance can be found on YouTube.
For creators, performers and audience members alike, storytelling enriches our perspective of the world in addition to bringing us joy. My advice for others is that if you see something you want to change, find a creative way to change it. The world is a better place when we’re not satisfied by mediocrity.

“You are never too young to make a difference.”
Anika Consul (she/her) | Co-Founder of (You)th Cook, Student at Nikola Tesla STEM High School Class of ’21, Rising Freshman at University of Washington, and Youth Ambassador at the Bill and Melinda Gates Foundation Discovery Center
I never imagined something like COVID-19 could happen. Initially, when schools closed, an extra-long spring break sounded like a dream come true for a high school junior. But by the end of March, no one knew what was going to happen.
Then I saw businesses close and a rise in unemployment and food insecurity. I knew I couldn’t just hope things would get better; I needed to actively work to make it happen. While baking virtually over FaceTime one day, my friends Anisha Karnik, Ananya Nandula and I came up with the idea of using cooking and baking for a cause.
That’s how our community service organization was born. Through You(th) Cook, we cook meals weekly and donate them to shelters in need across the Greater Seattle Area. We’ve provided over 3,500 nourishing, healthy and wholesome meals to The Sophia Way, Tent City, Helen’s Place, Congregations for the Homeless, the New Bethlehem Day Center and other homeless shelters across the Eastside of Seattle.
When it was announced that the 2020-21 school year was going fully online, we also reached out to elementary school teachers in the district and created a mini-baking curriculum to educate young learners about the science behind food through hands-on baking projects.
By starting You(th) Cook, I had the incredible opportunity to help others in need – and I learned how to mobilize my community during such an unprecedented time.
Its success only reinforced my belief that you are never too young to make a difference.
This work is important to me. I think of it like the domino effect – if you do something kind for one person, they’re likely to do the same for someone else. It creates a chain reaction of kindness. Seeing so many people reaching out through our initiative has been inspiring. It gives me hope that humanity has exceptional power to come together and conquer anything.
Website | (You)th Cook
Instagram | @you.thcook

Alyssa ©️ Jennifer Winter Photography
“The world put us online because they couldn’t handle us in person.”
Alyssa Jiwani (she/her) | Student at New York University Tisch School of Drama, Founder and Artistic Director of The Virtual Theatre Co, Overlake School, Redmond Class of ’20
I still cannot wrap my head around what happened in the last year. It feels like the world flipped upside down within weeks.
I was a graduating senior in the class of 2020 at the Overlake School in Redmond, Washington. The closing night of my senior musical was on March 8, 2020. It was my 19th and final show over the course of seven years. After that night, I never went back to Overlake again and I never got to hug friends or teachers again.
When the rest the school year was cancelled, I missed Overlake’s annual benefit concert, which I’ve led for the past few years. I decided to move it online to a huge, live-streamed concert benefitting Feeding America’s COVID-19 Relief Fund. I edited together performances from all of Overlake – 5th to 12th grade, faculty and alumni. We raised over $15,000 for COVID-19 relief. It was a heartwarming end to my time at Overlake.
Theatre and art got me through the trials and tribulations of high school, so when I heard from friends that their schools were canceling productions – and some schools were even defunding arts programs – I was horrified. I couldn’t imagine going through high school without that light.
Then I remembered how I put together the virtual benefit concert and realized that online theatre was a lot more plausible than people realized. I had a lightbulb then to create The Virtual Theatre Co (TVTC).
With its launch in July 2020, TVTC offers classes, productions and workshops. We have students from over 10 countries from around the world. Members of our creative team are working professionals in the theatre industry and theatre students from top-performing arts universities in the country. I run a workshop called Everything Broadway where we bring in Broadway stars, and students work with their inspirations. We’ve had Tony Award-nominee Taylor Louderman, TikTok star JJ Niemann, Wicked’s Jennifer DiNoia, Hayley Podschun, and DJ Plunkett, Mean Girls’ Mariah Rose Faith, Krystina Alabado, Kyle Selig, Cailen Fu, Frozen’s Caroline Bowman, Hannah Jewel Kohn and more.
One of our mottos is that the world put us online because they couldn’t handle us in person … and it’s true! Growing up, I was never represented on stage or on screen. I’m a young, short, tiny brown girl. I didn’t get opportunities handed to me, whatsoever – and I desperately want to change that for future generations.
Fighting inequity is the basis of TVTC, with its three main pillars to increase accessibility, inclusivity, and diversity. At TVTC, we are all trying to change the theatre industry for the better.
Theatre has the ability to be one of the biggest methods of change in our world. The younger generation of artists are coming in strong, and I’m excited about the future. Our generation is truly unstoppable.
Website |The Virtual Theatre Co
Instagram |
@thevirtualtheatreco

Ming-Ming © Bill & Melinda Gates Foundation/Alex Garland
“This was a community effort with one goal: To fight COVID-19.”
Ming-Ming Tung-Edelman (she/her) | Founder and Executive Director, Refugee Artisan Initiative
After 25 years of being a clinical pharmacist, I always wanted to give back to my community.
As an immigrant from Taiwan who came to the United States about 35years ago, I understand what it means to give a woman tools and skills to become self-sufficient and be financially Independent. My own grandma, a single mother raising three children as a seamstress inspired me that tools, plus skills can transform lives. Five years ago, I founded the Refugee Artisan Initiative (RAI). We employ refugee and immigrant women and train them in artisan skills and small-batch manufacturing so they can build better lives for themselves and their families.
The pandemic has been transformative for us. When COVID-19 first hit in March 2020, we were able to realize our strengths and pivot very quickly to provide what the community needed. Suddenly, sewing became a very valuable skill … to make masks, medical scrubs and face shields.
Since we are upcyclers with a lot of donated fabric – like, stacks of 100% cotton bedsheets, donated from California Design DEN – we had the best material to make masks to protect our community against COVID-19. I designed them in a day and put out our first GoFundMe campaign. Within two days, we raised over $10,000 then received a match of $10,000 from Rotary Club of Seattle NE. This enabled us to make more than 5,000 masks a week. A few husbands even helped! This was a community effort with the same goal: to fight COVID-19. We sent masks to postal workers – and across the country to New York and to the Navajo Nation which were hit hard by the pandemic. Partnering with Swedish Health System and their Community Health Investment we are making medical scrubs. All these opportunities allow us to hire more refugee and immigrant women coming to Seattle and using their sewing skills to make critical items while supporting for their families.
Living in a supportive community where people want to make a difference only motivates me more.
This year has shown human resiliency – and I hope it has also been a time of reflection. We can wear multi-layered masks and N-95s, but an actual vaccine can create immunity and stop the virus. That has given me a hope that we will come out at the end of the tunnel – and surprise ourselves by seeing that the sky is brighter and bluer.
– Told to Marcus Harrison Green, South Seattle Emerald, in April 2021
Get Involved |
Refugee Artisan Initiative
Instagram | @refugeearts
Facebook |
@refugeearts
Fighting and Treating COVID-19

©Bill & Melinda Gates Foundation/Charina Pitzel
“You cannot tell the story of disparities and inequities without telling stories of strength and resilience and power.”
Esther Lucero (she/her), President and CEO, Seattle Indian Health Board
Yá’át’ééh. I am Diné on my mom’s side and Latina on my dad’s side. Some folks are surprised when I tell them my first career was in the corporate world, where I achieved a lot of success, but I wasn’t giving back to my community. So I used that money and headed for med school, until I realized I was really interested in addressing issues grounded in systems. I soon fell in love with studying federal Indian law, so my graduate work was in public policy.
Now, I have the privilege of leading the Seattle Indian Health Board, a 51-year-old organization that operates as a Federally Qualified Health Center and Urban Indian Health Program, as designated by Title V of the Indian Health Care Improvement Act. We also have a public health arm – the Urban Indian Health Institute – that does research, epidemiology, evaluation, and data work. We’re uniquely positioned to provide direct-service healthcare, overall health and human services, residential treatment, and public health outreach. We’re part of the Indian Health Service system designed specifically for urban American Indians and Alaska Natives across the nation, but we serve all people, and we serve them in the Native way. We call our patients our relatives.
Meeting our own needs
At the beginning of the pandemic, I put in a request for personal protective equipment (PPE) from the Public Health department of King County. Instead of PPE, we received an anonymous box of body bags.
This may be shocking to people, but it’s not the first time that American Indian and Alaska Native communities have received this kind of response. Minnesota Representative Betty McCollum called to ask me about it, and I offered that maybe it was a mistake. She said, “It’s not a mistake. These things have happened intentionally.”
I think those body bags are a symbol that, to government systems, we’re not worth it – that we’re a cost, not a benefit. As American Indian and Alaska Native people, we have a unique relationship with the federal government, where the federal government owes us a tremendous amount of benefits and resources due to the secession of land. Depending on the administration, there have been attempts at eliminating that fiduciary obligation. It’s simply racist that people think of us in a way that doesn’t honor our strength, or the ways we come together to lead efforts, or our cultural ways of being and ways of knowing.
It has been a rare occurrence when we’ve been able to trust government systems, so instead we find trust within our own community.
Because we’re resilient, because we gather as a community to make sure that we are strong and move together, we pool our own resources. So, in relation to the pandemic, Louie Gong, who is part Nooksack and owner and CEO (at the time) of the lifestyle company Eighth Generation, donated $10,000 worth of PPE. Dr. Terry Maresca, one of our preceptors here at the clinic, rallied her medical students to bring in disposable and washable scrubs.
In the end, we wound up with more PPE than we could use and were privileged to donate it to other organizations that needed it.
Expanding the sphere of safety
As the pandemic continued, we had to change our whole service delivery model practically overnight. We went from 4,500 phone calls per month to 4,500 per day, so we expanded our data systems and staffed a call center. We moved in-person appointments to telehealth – and, for members of our community who don’t have access to cell phones, we created telehealth kiosks. To provide testing services, we acquired a machine to do onsite testing, which shortens the waiting time for results. We also amended our elders’ program so elders could continue to get a warm meal, visit with one another, get access to case management services – all without having to isolate from families and grandchildren.
We’ve had to come up with creative solutions to ensure that we’re there for our relatives who needed our services – and we did that while never closing our doors.
When vaccines became available, we couldn’t use the Pfizer vaccine because low temperature freezers were not available, so we decided on Moderna. We wound up being the first organization in the state to receive the Moderna vaccine, and I happened to be the first person in the state to receive the Moderna vaccine – it’s true! I wanted to show that I wouldn’t ask our community to do something that I wouldn’t do myself.
Due to the ingenuity and organizing skills of our staff, we were able to provide a thousand vaccines a day without wasting a single drop.
Through our public health arm, we worked with community- and youth-led panels to produce materials designed specifically to be understood by our communities. The 29 federally recognized tribes in the state of Washington allowed us to leverage their sovereign authority to implement testing and vaccination protocols, according to our community need. We started, much like the CDC recommended, with staff and elders. But we also expanded to our culture keepers, like our language speakers. We need to keep those folks and those epistemologies protected. 90% of all American Indians and Alaska Natives are vaccinated here in King County, which tells you how successful we have been.
We call our model “expanding our sphere of safety.” We prioritize the needs of the community, while at the same time building for a more far-reaching scope. We were so successful that the state of Washington even adopted our protocols, such as asking hospital systems to vaccinate staff from partner organizations. We also worked with community champions like Seattle councilmember Debora Juarez and Denise Juneau, then superintendent of public schools, to establish a collaboration with Seattle Public Schools to vaccinate special needs staff.
That’s what it looks like when the sphere of safety is empowered to expand.
Overcoming inequity
We face many barriers to equity – at the institutional and individual levels. Inequities are prominent in health outcomes and death rates. Our people have been hit hard. Folks experiencing homelessness or living in poverty may not be able to isolate or may not have access to PPE or hygiene products. Our undocumented relatives may be scared to seek services because they don’t know if becoming part of a national database could make them targets of ICE.
As a society, we already know how to overcome challenges of inequity. It takes two things: first, transferring resources and, secondly, transferring power.
There’s a lot to be angry about. At the same time, we’ve seen the largest investment in infrastructure than we will probably see in my lifetime. That offers a chance to escape that scarcity mentality and focus on economic opportunities. We have two additional clinics opening next year, and a dental mobile unit. Those things are massive!
But you cannot tell the story of disparities and inequities without telling stories of strength and resilience and power. At the Seattle Indian Health Board, we’ve learned what we’re capable of. We stand together in community – and we’re unstoppable.
We, as American Indian and Alaska Native communities, regardless of whether we live on our tribal lands, in our reservation systems, or in urban environments, are all tribal people, and we will always band together for the well-being of our communities. We are current and modern and innovative and smart and strong. Like our indigenous ways of being and knowing, many folks can learn from us and stop hoarding the resources. We’re still here. We’ll show you the way.
– Told to Thanh Tan, independent journalist, November 2021
Website | sihb.org
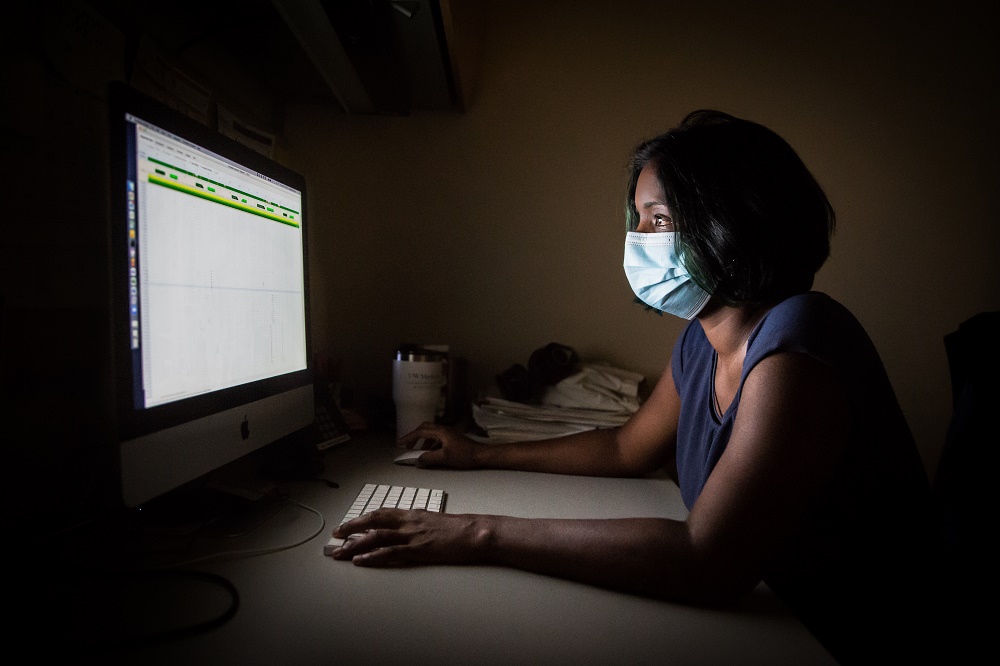
©Bill & Melinda Gates Foundation/Charina Pitzel
“We can’t deny we are globally connected.”
Pavitra Roychoudhury (she/her), Computational Biologist, University of Washington and Fred Hutchinson Cancer Research Center
I’m a computational biologist at the University of Washington and the Fred Hutchinson Cancer Research Center. My specialty is working with the genomes of viruses, which means analyzing the nucleic acids, that’s DNA or RNA, in a virus.
From the beginning of the pandemic, my colleagues recognized the need to sequence the virus. Before COVID-19, I was working with human herpes viruses, human immunodeficiency virus (HIV), and respiratory syncytial virus (RSV), so I was able to apply those skills to SARS-CoV-2 – the virus that causes COVID-19.
February 28th was the day the first SARS-CoV-2 test sample arrived in our lab. We put it on our sequencer as fast as we could and by the next day we had analyzed our first genome – “UW1”–which was the third genome for Washington state.
When you get tested, you’re given a nasal swab which is then processed for your test result. If it’s positive, we take that sample and use lab techniques, mathematics and computing tools to determine the genetic sequence – or genome – of the virus in that sample. Initially, there was intense interest in using genetic sequencing to understand if cases were from travel or local transmission – and if local, how much community transmission has there been? But even back in March 2020, we knew we were behind in this pandemic. We knew the horse had left the barn – and bolted.
Then, for a large part of 2020, we thought this virus was behaving in a somewhat expected manner, but towards the end of the year, we saw variants come out of the UK and elsewhere that were spreading rapidly. We realized we were flying blind here in the US because of how few positive tests were sequenced. When you hear about variants, it’s the genetic sequence of virus samples that gives clues into what might be happening. Different mutations might impact disease severity or infectiousness, or they might indicate if the virus is escaping vaccines. The new variants really made us focus on sequencing, to scale-up our efforts.
People used to say things like, “Why aren’t we sequencing more and faster?,” but the reality is that in addition to a lack of funding and support, a lot of us have experienced burnout. Since the start of the pandemic, we’ve worked hard while taking only a little bit of time off. Because our lab is a testing lab, we are considered essential workers. For all essential workers, a huge amount of credit needs to be given to families and support networks. For me, that’s my husband and my daughter. My daughter is five and she really gets it. That it takes a village––at work, at home, and in the community – to come together to fight this pandemic.
Vaccines have shown that they are the greatest tool in tackling this pandemic. Without the genetic sequence of the virus, we would not have been able to design the vaccines we have right now. And yet there are huge inequities related to vaccine availability and distribution and uptake. As community members, we need to see what we can do to convince those who are unvaccinated to get vaccinated. Sometimes people are quick to point the finger at the unvaccinated and say, “Oh, these people are just choosing to be unvaccinated.” But not all unvaccinated people are driven by misinformation; for some, there are barriers, including structural issues. Can people take time off to recover the day after they receive their shot? Have we created safe spaces for people to do that, or to bring up any concerns they have? Because a lot of them are valid concerns and I think there are many things that we can do to address some of these inequities.
There’s still more to be done to make sure we turn the corner with COVID-19. People should recognize that, when we talk about travel restrictions and all the inconveniences related to the pandemic, there are populations that are still vulnerable to this disease – here and globally. Let’s not forget children all around the world are still not eligible for vaccination. Because we are connected, outbreaks in all those populations will ultimately impact us, so we need to think beyond our local communities. That’s going to make a difference over the next few months in this pandemic – and in future pandemics.
What gives me hope is science and the speed at which we have been able to tackle COVID-19. It’s the result of a lot of people coming together, often at great cost to themselves, and taking on incredible amounts of responsibility. For this pandemic and any other pandemic, what’s needed is for us to come together and take whatever skills we have and put them to good use.
– Told to Marcus Harrison Green, South Seattle Emerald, in April 2021
Website | dlmp.uw.edu/research/centers
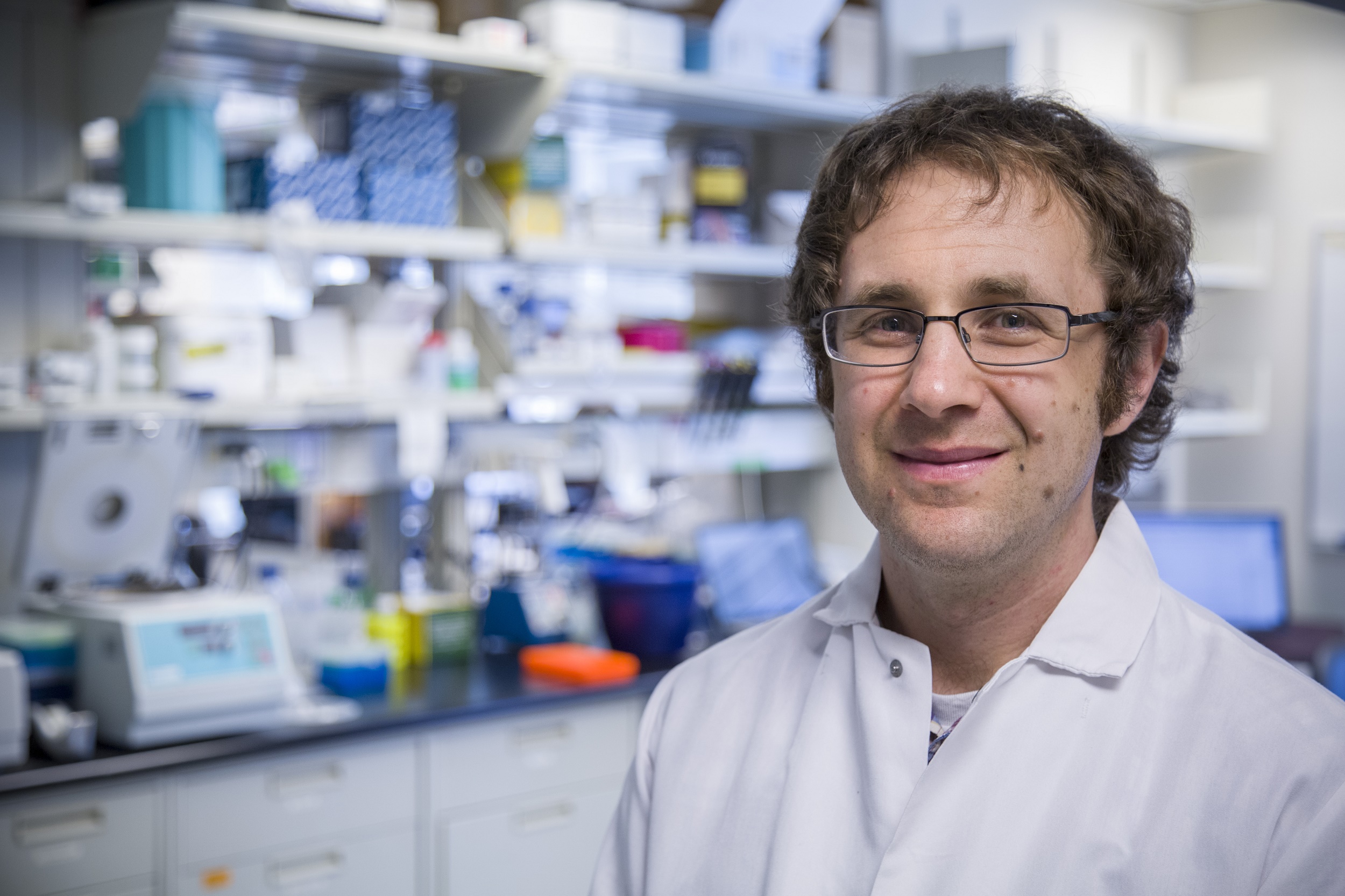
Jesse © Bill & Melinda Gates Foundation/Alex Garland
“When most people are vaccinated, this could be a lot less serious.”
Dr. Jesse Bloom (he/him) | Associate Professor, Fred Hutch Cancer Research Center, Affiliate Associate Professor, Genome Sciences & Microbiology, University of Washington, and Investigator, Howard Hughes Medical Institute
I was always interested in evolution and how things change. As a scientist and faculty at the Fred Hutch Cancer Research Center for 10 years, I now study viruses and how they evolve.
Prior to the COVID-19 pandemic, we studied a lot of viruses, including influenza and HIV (human immunodeficiency virus). When we started to hear reports of an outbreak in China, it was clear to someone who studies viruses that this was going to spread. It was then that I started to think about how we could switch our research to study the coronavirus.
Currently, my lab is focused on understanding how coronaviruses like SARS-CoV-2 evolve. This helps determine if immunity will be long-lasting or not. With some viruses (like measles), people are protected for their entire life once they get a vaccine or infection; for others (like influenza), the virus evolves and is eventually able to re-infect. Common cold coronaviruses evolve to erode immunity, which is part of the reason that people are re-infected every three to five years.
One challenge I faced during the pandemic was that the research needed to be done quickly and everything mattered. But knowledge only goes so far and must be combined with action – which explains in part the despair many felt from the government’s overall response. Now the concern is that people should have access to the vaccine – and actually take it.
I don’t think COVID-19 is going away. And yet, while I don’t think we’re going to be able to totally stop thinking about it, it could be a lot less serious once most people are vaccinated. The virus’ transmission could be cut down a lot, and there will be a lesser risk for getting really sick.
People are working very hard on this. To be at the forefront in helping people understand this virus, as a scientist, has been really rewarding for me. I feel like I’m doing stuff that matters, that makes a difference – something that people care about.
This time has drawn out how important different contributions are to keep the society functioning, from doctors and nurses to first responders and essential workers. It makes me really appreciate how all of society needs to click together to make it through something like this.
– Told to Marcus Harrison Green, South Seattle Emerald, in April 2021
Website | Fred Hutch Cancer Research
Center
Facebook |
@HutchinsonCenter
Instagram |
@fredhutch
Twitter |
@fredhutch
News | Dec.
2021:
New York Times
Editorial
by Jesse Bloom on the Omicron
variant.
Spreading Joy and Healing

Linda © Jacy Watson
“I realized the importance of creating third spaces – spaces outside of home and work that are nurturing and accessible to all.”
Linda Yan (she/her) | High School Senior at Bellevue High School, Intern at Northwest Folklife and Penguin Productions, Co-President of Model United Nations Club
March 2020 feels like a month and a lifetime ago. When news broke that we weren’t returning to school anytime soon, I was paralyzed. As a high school senior deeply interested in STEAM (science, technology, engineering, art, math) who’s also the captain of my school’s cross-country team and co-president of our Model United Nations (MUN) club, I found my daily routine completely upended by the COVID-19 pandemic.
Aside from extracurricular activities, my average school day was reduced from seven hours to three – and this new reality wasn’t going to disappear in a few weeks. I was suddenly left with a lot of time that I needed to fill.
Along with many young leaders in my community, we knew we had to pivot. I began working for nonprofit organizations like Helpful Engineering, a global open-source medical device incubator, and Penguin Productions, a Seattle-based youth-led theater company run by Northwest Folklife.
It’s important to me that I create what I want to see in my community. With many of us experiencing alienation and loneliness during this time, I realized the importance of creating third spaces – spaces outside of home and work that are nurturing and accessible to all.
We began experimenting with several platforms to find one that suits our needs to host virtual MUN conferences. I find it incredibly empowering for adolescents like me to discuss and seek solutions at the MUN for critical world issues like climate change and the global refugee crisis.
Whether it’s at a cross-country race or a MUN conference, I love seeing joy in people’s faces. Witnessing the world persist and abide, despite all the tragedies that are occurring every day, is something that gives me lot of hope.
I’d like to believe that a lot of the things that we miss, such as hugging loved ones and going to the theater, are simply wintering, and that we will (hopefully soon) dust off the snow and enjoy them once again. At the end of the day, I think my greatest accomplishment this past year has been simply surviving.
Website | Northwest Model United
Nations
Facebook | @NWMUN
Instagram | @nwmun

“We believe it’s the little things that count.”
Ayla Karmali (she/her) | Junior at Newport High School, Co-coordinator of Greater Seattle Acts of Random Kindness
As a busy high school student, my days were packed with activities – but when COVID-19 hit, that all stopped. I began reflecting on what really matters in life. To me, that was connecting with people.
It became clear that, because of the COVID-19 pandemic, many people didn’t have moments of happiness or connection with others.
In June 2020, we founded the Greater Seattle Acts of Random Kindness (ARK). My team and I reflected on what our community needed most during this time. With a lack of connection and community due to remote working and online learning, we made it our mission to give our community a sense of joy that so many of us were lacking.
We believe it’s the little things that count. We’re currently working on a project called “Chalk the Streets: Spread Kindness through Art.” We set up chalk in baskets across Bellevue, encouraging people walking by to draw or write something that makes them smile.
I love that that you don’t need a lot of money to do something joyful.
We’ve also facilitated the creation of multiple ARK clubs around Seattle, whose members have made cards for senior centers, healthcare workers and people experiencing homelessness, and notes and gifts to encourage teachers and students during this isolating time.
Through the Greater Seattle ARK projects, I see the smiles we put on faces within our community. I like to think that for every smile, there is someone who might be empowered to achieve something new or find strength to power through one more day.
Website |
Greater Seattle Acts of
Random Kindness Club
Instagram |
@greaterseattleark

Rhea ©️ Shweta Kulkarni
“Art became my outlet to express this change.”
Rhea Kulkarni (she/her) | Student at Skyline High School, Founder of The Photo 4 Good L.L.C, and Youth Ambassador at the Bill and Melinda Gates Foundation Discovery Center
COVID-19 has made me aware of the disadvantages and inequalities of opportunity people face. While staying home and quarantining, I had time to learn about and reflect on those most affected by the pandemic.
The burden of disease is never equal in society.
Living close to Seattle—the third most homeless-populated city in the country—I saw the epidemic first-hand throughout our streets. I saw people experiencing homelessness were at a greater risk of contracting the virus.
I wanted to work towards changing it, and art became my outlet. I realized that art—and photography, in particular—can bring awareness to how the homeless epidemic that my community faces was especially impacted by the pandemic.
I founded The Photo 4 Good L.L.C. in the spring of 2020 to contribute to and foster a safe environment for the homeless youth community in Seattle through art. When you purchase art on the site, all profits go to Teen Feed, a Seattle-based nonprofit shelter for homeless teens that provides youth with basic needs – healthy meals, access to healthcare and street outreach.
My photographs are a way to express myself and bring awareness to the importance of art in social activism. Because of the intersectionality between artwork and activism, art can be a means to help our homeless communities.
While I am grateful for the opportunities I have for a successful life, I believe every child, regardless of their upbringing, deserves this too.
Website | The Photo 4 Good L.L.C.
Gates Foundation Staff and
Grantees

©Bill & Melinda Gates Foundation/Charina Pitzel
“We’ve got a better system now that better protects people for whatever the future holds.”
Scott Dowell (he, him), Vaccine Development & Surveillance – Surveillance and Epidemiology, Bill & Melinda Gates Foundation
My role at the Gates Foundation is leading our COVID response. It started as an ad hoc pandemic preparedness group that was meant to be part-time – but since March 2020, it’s been COVID, COVID, COVID.
I’m a pediatric infectious disease doctor by training and an outbreak epidemiologist. My “day job” has been focused on understanding the causes of childhood mortality. I was with the U.S. Centers for Disease Control and Prevention (CDC) for 20 years – and I came to the foundation during the 2014 West African Ebola outbreak. Since then, I also worked in the Zika outbreak and the North Kivu Ebola outbreak.
This is by far the biggest epidemic any of us have experienced in our lifetimes.
Getting involved
I think the foundation got into the
business of outbreak response
somewhat deliberately.
Philanthropic foundations are not often thought of as critical to outbreak response. It’s traditionally the responsibility of governments to protect populations against threats, whether that’s aggression from other countries or health security risks from epidemics. But foundations can play a catalytic role. We have the freedom and flexibility to risk money on things that might fail.
It’s something that Bill [Gates] and others had been talking about for several years. They noticed, “One of the most significant threats to society and humanity comes from natural pandemics, and we’re not paying enough attention.” Back when the West African Ebola outbreak was growing, the foundation was among the first to say, “Hey, this is a serious problem that’s not adequately addressed by governments. We’re going to put fast, flexible funding towards things that can help, like frontline responders and new, high-risk innovations for diseases that affect the world’s poorest countries who are often ignored.”
In late 2019, when we first heard about the new coronavirus, investigators in China had already sequenced the virus and shared that sequence. That happened very quickly, but there still wasn’t much information. We knew it was a new coronavirus in the SARS (severe acute respiratory syndrome), beta coronavirus family. We had experience with the Middle East respiratory syndrome (MERS) and SARS 1, so we knew this new virus was potentially bad – and we knew it was severe enough that health workers were being hospitalized, which is pretty unusual.
We started to think person-to-person transmission could be occurring, even if it wasn’t acknowledged yet. The first evidence that it was spreading beyond Wuhan came in January from a case identified in Thailand … and then another in Japan. I remember sitting with my colleague Keith Klugman – director of the foundation’s pneumonia program and expert on the 1918 flu epidemic – calculating how many people travel from Wuhan to Thailand and Japan. We asked ourselves, “How many people are missing from this picture?” And we realized it’s not 20-some; it has to be tens of thousands of cases to have these 20 confirmed cases. It became more and more clear that this was a highly transmissible human-to-human pathogen. It ticked a lot of boxes – those red flags that determine if something is a real pandemic threat.
I’ve done many outbreak responses in the past, and the fundamentals are not all that different. You need to get money out to the front lines. People need to collect data to solve the principal questions – how transmissible is this thing, and how severe is it? Both of those answers determine whether vaccine companies will be willing to start investing in vaccine development – and whether governments are going to take it seriously.
In those first few weeks, we started thinking, “Looking at therapeutics, diagnostics, vaccines, and so forth, where do we risk investing?” Right away, we came up with nearly US$ 50 million worth of potential investments. Then my colleague Anita Zaidi, president of the foundation’s gender equality team said, “Given how big this is, if we’re right, we should double the investment.” So, we put together US$ 100 million worth of budget and went to Bill and Melinda. They said yes, and we were off.
Early on, years earlier, we spent time and money on therapeutics and diagnostics and – fortunately – in mRNA vaccine technology. One of the biggest successes, outside of public health measures, was just how fast and how effective mRNA vaccines have been.
The importance of public
health
To me, one of the most remarkable
things about the COVID pandemic is
just how effective nonpharmaceutical
interventions have been. I
don’t think people appreciate
how many lives have been saved
because of public health suppression
measures – by masking, closing
schools for a while and limiting
travel. Those are some of the first
things you think about because you
can do them right away, and they can
slow down transmission.
When those things have been done in small ways in previous outbreaks, there was a lot of blowback. Given the way people raged about school closures in New York over H1N1 influenza, no one in public health would have predicted that these current mandates would have been put in place as robustly as they have.
The World Health Organization estimates that 80,000 to 180,000 healthcare workers worldwide died from COVID between January 2020 to May 2021. That’s awful. These are the people who are taking care of everybody else. That has to be one of the most frustrating and challenging things for people working at the foundation.
To see poor countries left so far behind from lifesaving vaccines has also been frustrating and challenging. As the majority of populations in Europe and the U.S. are becoming fully immunized, if you look across African countries in the same time frame, vaccination rates stayed below 25%, with some as low as 1-2%. The vast majority of people in African countries having not been protected by a vaccine, while in rich countries we’ve enjoyed access to vaccines for many, many months. But even here in the U.S., poor communities and communities of color have been disproportionately affected by COVID and, to a lesser extent, by the lack of vaccines.
There are people who study health inequities, and finding a solution can be complicated … but at its most basic level, it’s money. The vaccines have gone where the money is, since the companies that make the vaccine are beholden to shareholders. Outside high-income countries, the COVAX Advanced Market Commitment buys vaccines, using donor funding, for low-income countries that cannot otherwise afford them. All the while, though, rich countries are saying to vaccine manufacturers, “Put us at the front of the line. We’ll give you double, we’ll give you triple.”
There are some additional complexities, like manufacturing plants. Vaccines are manufactured largely in India, the U.S, Europe, and a few other places. There are almost no vaccine manufacturers on the entire continent of Africa. If we have a global system where vaccines are distributed more equitably, they could be manufactured in African countries and therefore directly distributed. This is a long-term goal and could be one of the solutions.
We are all connected
One lesson we’ve had is about the
interconnectedness of the world. An
event in Wuhan has an effect on
Seattle in a very short period of
time. The virus doesn’t
respect borders, and variants are
going to continue to emerge as long
as viruses can circulate and mutate.
When the Delta variant was first
recognized in India, it didn’t
stop with India; it went everywhere,
as we know.
I believe people are beginning to recognize our interconnectedness in a visceral way and I hope people come away with a gut feeling that this matters, because next time our lives will once again depend on it.
A lot of long-overdue public health advances are leaping forward – not just vaccines and therapeutics, but also our ability to do public health, like collecting disease surveillance data. These advances will guide and inform our responses. All of this has improved, and it’s not going back. We’ve got a better system now, that better protects people for whatever the future holds.
– Told to Thanh Tan, independent journalist, September 2021

©Bill & Melinda Gates Foundation/Shawn Koh
“We cannot do this as an individual team or country. We have to work together.”
Anna Du, 杜珩 (she/her), Senior Program Officer of Vaccine Programming, China Office, Bill & Melinda Gates Foundation
I’m a virologist with a background in pharmaceutical research and development and public health – and I work with the foundation’s vaccine development and delivery programs.
I would never have imagined everyone talking about technology and innovation in vaccine development like they are now. The foundation had a lot of experience before COVID-19, and the pandemic put our knowledge to use like never before.
There are a lot of challenges to my work – but I love my job. In my role, I support partnerships to help Chinese vaccine companies prequalify for approval by the World Health Organization and coordinate supply through Gavi, the Vaccine Alliance. I also work on vaccine delivery, which gets the vaccine to people and ensures everyone has equitable access. The third part of my job is using a technical approach to innovation to reduce the costs of goods. Many people think new technologies increase costs, but they actually help increase capacity, which then reduces costs. Lastly, I also look at how we can support Chinese vaccine industries to supply more volume to low- and middle-income countries, to increase vaccine access worldwide.
Responsive expertise
Things really changed for me at the end of January 2020. At the time, I was in Seattle to discuss vaccine strategy with colleagues when we got the news about the COVID outbreak in Wuhan. Two days later, I was calling a face-to-face meeting at the foundation with epidemiologists and vaccinologists. It was a very small team, just 10 people. Because I was from China and I have an infectious disease background, I participated the meeting.
Within a week, I was appointed to lead emergency response out of the China Work Stream, which meant I had to figure out our strategy to implement the response immediately.
I’m trained in vaccines, but before we could think about vaccines, we had to work on diagnostics, therapeutics, and epidemiological modeling. Working with the best scientists and scholars across disciplines was amazing. It helped me learn a lot about virus movement and pandemic response.
I also helped connect Chinese scientists with the Coalition for Epidemic Preparedness Innovations (CEPI). Early on, CEPI sent out requests for proposal (RFPs) for COVID vaccines. At that time, Chinese scientists were not familiar with CEPI, so I told them about the RFP. Some of them applied, and a few were brought on board. That’s an example of how I build connections between China and global vaccine networks.
On a more personal note, I stayed with my mom for the first 10 months of the pandemic. Because I’m a virologist, I was able to advise her on how to suit up in personal protective equipment, so she could go pick up deliveries and groceries for the whole family. She felt honored to do that because it meant she was protecting us. While I was there, I missed being in the city and seeing friends, but she cooked for me, which allowed me to work around the clock.
Within those 10 months, a vaccine was developed. Timelines for vaccine development usually take 10 to 20 years. In all my previous vaccine development work, I have never seen a vaccine from start to finish. It moved fast precisely because of all the effort, talent, and technologies that went into vaccines for HIV, tuberculosis, and malaria – even innovations like mRNA technology and clinical studies. It was really encouraging. In a short period of time, we pooled experts, scientists, scholars – people from a variety of fields. An incredible amount of solidarity went into COVID vaccine development. We also mobilized unprecedented financial contributions. It’s incredible to have a whole-of-society approach to coordinate and cooperate on getting to a vaccine.
Cooperative innovation
The next step for COVID is to look at how we can support a vaccine candidate to pass stringent safety and efficacy tests and supply low- and middle-income countries, which haven’t had vaccine access. At this point, my job is to accelerate the scale up and delivery of those vaccines which have met the safety and efficacy requirements. We’re facing actually too many vaccine candidates and technologies now, and our resources are limited. The question has to be, which vaccines will serve people best – and most quickly?
As foundation staff, we always think about what we can do to advance equity in vaccine access and other aspects of global health. How to approach an issue, what caused it, and how to find a solution – that’s our job. Everyone at the foundation is a goalkeeper. We feel a strong sense of responsibility and urgency to do the job right. And we can harness the energy of this moment.
The work we’ve done during the COVID pandemic will contribute to other pandemic responses. It will contribute to work on other vaccines for HIV, tuberculosis, and malaria – or access to vaccines like the HPV vaccine, which has a shortage.
I believe that science, innovations, and good solutions can fill the gaps in society, but we need to be more collaborative. We need to explore a cross-disciplinary model of collaboration. Even if we’re disconnected due to travel bans, we’re one team. You can look at vaccine development as one whole group – we call it the “immuno-society” or “immuno-community.” We cannot do this as an individual team or country. All of this vaccine expertise must come together as a whole. We have to work together.
– Told to Thanh Tan, independent journalist, September 2021

©Bill & Melinda Gates Foundation/Charina Pitzel
“Public-private-community partnerships are crucial. They help us not only respond to a crisis, but also build more resiliency in our society.”
Toni Hoover (she/her), Director of Strategy Planning and Management for the Global Health Division, Bill & Melinda Gates Foundation
I led Pfizer’s largest research and development laboratories before joining the foundation in 2012. I could see then that the foundation had impact in the world and would continue to in the future. Now, I’m the Director of Strategy Planning and Management for the Global Health Division at the foundation. Among other things, my team is responsible for product development portfolio management within the Global Health Division. We track the development and delivery of products we invest in, including vaccines, drugs, diagnostic devices, and vector control agents like insecticide-treated bed nets to fight malaria. For every product that starts as an idea, it goes through rigorous research and development by our partners to determine if it’s safe and effective. Then, we work with our partners to ensure it can be manufactured, commercialized, and get delivered to those who need it most. Finally, every product needs approval by regulatory authorities, including the World Health Organization.
The foundation has audacious goals, including goals to eradicate diseases. Just prior to my decision to join the Gates Foundation, India had been declared polio-free. My father had polio, and, as a child, I heard stories about how polio affected his life.
I thought at the time, maybe I would be able to take my learnings from product development and apply it to diseases of the poor. Maybe my 25 years in the pharmaceutical industry were preparing me for this moment to join the Bill & Melinda Gates Foundation.
Purpose-driven work
The COVID-19 pandemic was one of those moments when I realized this is why we do the work we do. It’s to be able to fill a critical role with everything from innovations to delivery systems … because this is the work that needs to be done in a pandemic so everyone has access to life-saving tools, and not just people in high-income countries.
In early 2020, we could see the pandemic coming through modeling done by the Institute for Disease Modeling and the Institute for Health Metrics and Evaluation at the University of Washington. We had just completed our annual strategy review period, which is a seminal moment in the rhythm of life at the foundation. But then, everything changed, and our leadership decided it would be best for us to work from home beginning in early March 2020.
Improving health outcomes in a health emergency
Because of my connections in the pharmaceutical community – and in communities of color in the U.S.– two of my peers brought me in on a separate project. It was a public-private-community partnership in the U.S. that included a consortium of researchers who were conducting clinical studies on the efficacy and safety of a therapeutic treatment for COVID.
Therapeutics are critical in public health emergencies – like the Ebola epidemic and now the COVID pandemic. So, we began looking into a therapeutic called convalescent plasma. With convalescent plasma, you utilize plasma from an individual who has developed antibodies to a particular virus as they recover. It’s a kind of therapy that can help someone who has just contracted the disease to jumpstart a generation of antibodies, with the hope that it increases their chance of survival.
I led a community engagement committee comprised of U.S.-based volunteers from multiple sectors and participated in the steering committee, which met weekly with Operation Warp Speed. We made direct appeals to the public to donate plasma. We had public service announcements from Dwayne Johnson, Helen Mirren, Samuel Jackson, Awkwafina, and others – but that wasn’t enough. So, we worked with community organizers and community leaders. We also worked with diagnostic testing companies that sent out notices to people testing positive to COVID to ask them to consider donating plasma upon their recovery.
The idea was that convalescent plasma would provide a bridge to the development of hyperimmune globulin (a concentrated form of antibodies), that then contributes to the development of synthetic monoclonal antibodies – which could ultimately help manage the pandemic until vaccines became available. Monoclonal antibodies were shown to be effective in treating individuals with COVID in the first few waves – and pharmaceutical companies now manufacture different antibody treatments that are routinely monitored to assess efficacy against COVID variants.
Lessons for the future
We learned a lot of important lessons about working with communities during this pandemic.
First, it’s hard to mobilize during a pandemic because people are just trying to stay alive. If you’re an essential worker, if you don’t have childcare, and if you don’t have access to healthcare, life in normal times is hard enough – let alone during a pandemic.
Then, as monoclonal antibodies became available, we learned that communities of color in the U.S. didn’t have the same access as white communities and especially high-income communities. The pandemic affected American communities of color disproportionately in terms of cases and deaths – but also life expectancy. Because of COVID, by early 2021, African American men had lost an average of three years of life expectancy relative to slightly under a year for white men, as just one example.
At the foundation, we’re taking lessons from COVID and applying them to our strategies in global health. But we also have to ask: how can we and others leverage what we’re learning in low-income countries and apply them to improving outcomes for the underserved in the U.S.? There are many similarities between the health conditions of individuals in low-income countries and individuals within a low socioeconomic status in the U.S., especially in communities of color.
Our aim at the foundation is to be a catalyst and help organizations find solutions that will work in their context, based on their experiences. These public-private-community partnerships are crucial. They help us not only respond to a crisis, but also build more resiliency in our society.
I’m never surprised by what a group of highly motivated and highly connected individuals within a community can accomplish. The ingenuity and innovation! You never know where a new idea is going to come from … but we know it will be needed. One thing is certain about what we’re experiencing: this isn’t going to be the last time.
–Told to Thanh Tan, independent journalist, September 2021

©Bill & Melinda Gates Foundation/Charina Pitzel
“We’re now in a place where we can think about what we’ve learned – and use that information to better plan for what’s ahead.”
Emmanuela Gakidou (she/her), Professor of Health Metrics Sciences at the Institute for Health Metrics and Evaluation (IHME), University of Washington
The common thread throughout my career is my interest in analytical or quantitative challenges. I am trained as a quantitative methodologist, working with health measurements from data collection on tobacco use to underestimates on death tolls during a crisis.
I never thought I would be doing quantitative analysis on an emergency basis, in real time, for presidents, heads of state, and Ministers of Health. I grew up in Greece and I was always good at math and interested in science. After I discovered the field of public health, where math and statistics apply to population-level problems, I got more training in statistics and other quantitative methods, plus epidemiology.
Solving for the unknown
Since the emergence of COVID-19, I have focused on modeling its impact and trying to forecast what might happen in the future.
Everybody on our team dropped what we were doing to focus on COVID. Initially, we were in crisis mode 24/7. It was “all hands on deck.” The scope of what we’re trying to do is so large that there is no way any single individual could do it on their own. The analytics we do with statistical modeling cannot even be run on a strong personal computer, so we use a supercomputer – the computational cluster – for all of our analysis. We also use a lot of data visualizations, and we have people look at everything on a regular basis for a “sanity check” to make sure the results make sense.
During the pandemic, we’ve seen a lot of fluctuations in data and data reporting. Assessing data quality is probably the hardest, most time-consuming thing we do as it cannot really be automated. We look at data as a team and then try to figure out whether an increase in cases might be a true trend versus a data reporting error.
It takes a lot of science and a little bit of art.
As the pandemic has progressed, more information became available about what was happening and what was needed. We’re now in a position where we can think about what we’ve learned, in terms of what have been effective strategies to mitigate the impact of the virus, both on health and on society more broadly. We can use that information to better plan for what’s ahead, whether it’s another wave or how to safely keep kids in school.
There are a lot of lessons from many months of data from 200 countries – and a lot of potential for data to shape public policy.
We draw upon these data when we advise governments. Whenever there has been controversy about what works and what doesn’t work to mitigate impacts of the pandemic or curb transmission, we’ll show data – for example, from places using masks to places using fewer masks, like we did in Poland. Mask use was low there until we were able to demonstrate with data the impact that masks can have and then the government implemented a mask mandate. Then, transmission went down. Having an impact like that motivates you to keep working.
Equity matters
Another lesson is how the pandemic equalized some things – but also brought out inequities in other ways. If somebody gets severely ill in a high-income country compared to a low-income country, they have access to very different levels of care. Of course, this was true before the pandemic … but the pandemic has brought to light some of the inequities that existed in health systems, both within countries and across the world.
One inequity not often discussed is in access to education. Education is a human right and a major social determinant of health, so it’s important to monitor the pandemic’s impact around the world, particularly for girls in societies where we had finally made progress in decreasing the educational gender gaps. We risk going back in time and perpetuating or worsening disparities that were previously there. There is still room for intervention to prevent this from having a long-term impact on society. Here in the United States, early results indicated large racial disparities in access to online learning and the quality of education. Around the world, there is a large inequity in access to online learning between high-income countries and low- and middle-income countries, and within low- and middle-income countries between the more wealthy and the less wealthy families. Schools in many countries also provide nutrition for children by giving them free meals, so the impact of school closures is more than just about learning.
Access to vaccines and antivirals is another obvious inequity. In higher-income countries, we’re so fortunate to be able to vaccinate children, and get boosters. But meanwhile a lot of my collaborators and colleagues are in other countries – India, Brazil and Indonesia – where people have access to less effective vaccines and large fractions of the population have yet to get their first dose. It’s upsetting to think about dosage waste that occurred in higher-income countries while there were people who would be so grateful to have these vaccines. As antivirals are emerging as an effective treatment, there is an opportunity for the global community to invest in sufficient production and equitable distribution.
COVID brings to light one manifestation of the unfair imbalance in global access to lifesaving interventions. We can hope that highlighting the urgent need for a better global system that distributes lifesaving interventions in a more equitable and efficient way will actually result in meaningful improvements.
I think we’re at a point where the inequities are hard to justify or to live with. Our motivation to work in public health is to decrease health inequities and improve the health of the most disadvantaged populations. These inequities are avoidable and the time to address them is now.
The human variable
Aside from work, one of the lessons I’ve learned during the pandemic is that you’ve got to seize the day. As soon as I am able, I know I will see my mom back in Greece – I haven’t seen her in almost three years. I’ve learned that when you have those opportunities to be with your loved ones, you must make the most of them.
I’ve also learned that it’s hard to predict human behavior. Even when there isn’t a knowledge gap, even when there are effective interventions, it’s hard to know how people in a particular location will react to a new development, a new variant, a new vaccine, whatever it may be. If there are any insights we can gain on how people might react in future health crisis, that would be important.
Overall, we need to fill data gaps. There are large geographic areas of the world where we have very little information. Even in places where we have information, very little of the data that we get is disaggregated by gender and other important dimensions. I would love us to place more value on collecting good information on health and wellbeing so we can make the best, evidence-based decisions in real time around the world.
– Told to Thanh Tan, independent journalist, September 2021
Website | healthdata.org

©Bill & Melinda Gates Foundation/Kris Connor
“COVID did not create inequalities, COVID exacerbated them.”
Micaela Iveson (she/her), Policy and Projects Manager, ONE Campaign
My dad was a Ground Zero volunteer at 9/11. He raised me to believe that, if you see a crisis, you run towards it and do everything you can to help. It’s because of him that I first came to understand that we are all connected – and all of our successes, and indeed our survival, are hinged on each other.
I’m a development professional with the ONE Campaign, an advocacy organization that works towards a very specific goal of sustainably ending extreme poverty and preventable disease by 2030. That goal has been severely set back by COVID-19.
I’m currently based in Washington, DC, with a crack-shot team that spans North America, Europe, and Africa. Our job is to use inarguable data points to sound the alarm on gross inequities, particularly in Africa, and make those issues feel personal and urgent, particularly to the average American, Canadian, or European. Increasingly, we work to elevate the voices of African organizations and individuals, ensuring that leaders in G7 countries are listening to African experts about what African countries need.
Numbers don’t lie
I manage our African COVID-19 Tracker, which we began in order to collect key data points that can help decision-makers understand what’s happening on the African continent in relation to the pandemic. We also have Aftershocks, a newsletter that communicates the social, health, and economic consequences of the pandemic throughout Africa. The purpose behind the Tracker and Aftershocks is to make these stats famous – to shine a light on stark injustices.
One of our most important data points is that, as of mid-January 2022, only 10% of people across the African continent were fully vaccinated. Compare that to over 70% in a lot of G7 countries.
Another way to look at it: for every person receiving a booster shot somewhere on the African continent this January, over 800 are administered in a wealthy country. Think about the implications. The best, emerging science says that people need booster shots to protect against Omicron, and 13 times as many booster shots have been given in rich countries than first shots have been administered in low-income countries. Thirteen times as many boosters as first shots.
Another example: just 150 out of 2000 clinical trials for COVID treatments take place in Africa, which significantly limits the continent’s capacity to access approved medicines. It means that many of the medicines that are used on the African continent haven’t actually been tested for their large-scale efficacy. And, since 90% of people are unvaccinated, they need more and better therapeutics than are available to a country like the United States – therapeutics which African countries don’t have.
A flashpoint in human history
Without a doubt, COVID is one of the greatest crises we’ll face in our generation, precisely because the inequity goes beyond the disease itself. COVID did not create inequalities; it exacerbated them.
Before the pandemic began, almost half of all African countries were at risk of being unable to pay off their debts. Since the pandemic, African government revenues have significantly declined, while at the same time the need for public spending to protect lives and livelihoods has skyrocketed. Advanced economies spent upwards of 18% of their GDP to protect their economies in 2020, while low-income countries with limited fiscal space have spent less than 2%. Recent reporting from the World Bank and the World Economic Forum show that the world economy will only become more unequal as a result of the pandemic. The projected global economic growth rate in 2021 was 5.5%, and it’s projected to shrink to around 3.2% by 2023.
This all has far-reaching consequences. For school children who lack access to computers or educational tools, learning losses during COVID-19 could cost this generation of students close to $17 trillion in lifetime earnings. Ten million girls worldwide are at risk of child marriage due to COVID-19. And that’s just a short list.
Equity takes all of us
Part of the ONE Campaign’s work is to hold leaders accountable for getting vaccines, testing, and treatment everywhere in the world.
There have been some efforts to take a global view. Early in the pandemic, the World Health Organization, the Coalition for Epidemic Preparedness Innovations, and Gavi began an incredible financing facility called COVAX. Its mission was to be the world’s clearinghouse for getting every country at least 20% vaccinated. Regrettably, rich country governments worked outside of the COVAX system to push themselves to the front of the line, ahead of low- and middle-income countries. Those rich countries ended up having billions of surplus vaccine doses and weren’t really sharing or deploying them. It’s a flawed system that COVAX was trying to fix.
COVAX has now distributed more than 1 billion vaccines and is leading the way for a lot of rich countries to mobilize and distribute millions more doses. But it can’t just be global agencies calling for change. Businesses and civil society have a role to play. I like to say to pharmaceutical companies, “Why can we get a cold soda in every country in the world, but we can’t get a vaccine to every person?”
The private sector must leverage its expertise and network to catalyze a global response, and – I cannot say this loudly enough – listen to African experts and policymakers for what they need in their own countries.
This is not about charity. It’s about justice and equality.
– Told to Thanh Tan, independent journalist, January 2022

©Bill & Melinda Gates Foundation/Mansi Midha
“When I spoke about vaccination, the women understood.”
Asha Kumari (she/her), JEEViKA, Bihar Rural Livelihoods Promotion Society, Bihar, India
I work in health, nutrition, and sanitation in Bihar, India – in the Garhpura block in the Begusarai district. I run trainings for community health workers in villages as part of JEEViKA, an initiative of the Bihar government that empowers rural women by mobilizing them into self-help groups to improve their physical health and financial well-being.
The work we do at JEEViKA means women and their children remain healthy and get a chance to move forward in life.
I’ve learned so much from being a part of JEEViKA and I continue to share these lessons with women in my village – young girls, teenagers, pregnant women, and mothers. Many lessons are about water hygiene and food diversity. Low-income women can’t afford all the food groups needed for healthy growth and development, so we advise them on how to grow a poshan vatika (nutrition garden), which arranges a variety of vegetables in a small piece of homestead land. We cover a range of health issues: from how to use sanitary napkins, to how to register for prenatal and birthing care, to when mothers should supplement breastfeeding with solid foods.
JEEViKA-promoted self-help groups provide their members, who are primarily women, with money to invest in their livelihoods as a loan they can pay back very slowly. It’s been critical because many banks don’t lend to individual women and demand collateral. But banks will lend to self-help groups, wherein the collective savings and the financial discipline of the group act as collateral. In our society, we women are commanding respect because of this initiative.
We have always tried to do everything we can to help people stay healthy and independent through community health education and financial empowerment. But, since the beginning of the COVID-19 pandemic, our work as trusted members of the community has expanded to provide guidance for many more urgent needs.
When the pandemic started, we were in a strict lockdown. Many of us were scared to leave our homes. There were rumors going around about the virus, so we knew we had to find ways to connect people with the right resources and factual guidance. We moved around the village using small side streets and by-lanes, knocked on windows, called on the phone – whatever we could do to battle misinformation and stress the importance of washing hands, wearing masks, and observing social distancing.
I wanted the women of my village to be well-informed so that no one would get sick. They had been working so hard to help their families get ahead, and I didn’t want them to face more setbacks. That’s when I started to spread the message myself. At first, my family was scared for me to go outside – and I was scared too. I even scared the women I was visiting, who wondered why I was there.
It took some time and effort before the women started to listen. But because of the lockdown, and because people had no means of transportation, they were running out of food. I was already in touch with women in the village to help them with their ration cards and help ensure food security, which opened new lines of communication. I told them that everybody was scared – and I was no exception – but we needed to protect our families by having the correct information to stay safe and get the supplies we needed to survive. I gave them tools to do that, which instilled confidence in them. I also heard women were having trouble sourcing sanitary napkins during the lockdown, so I spoke with a shopkeeper to ensure a steady supply. Then I informed the women that they could find supplies at this particular store, which in turn helped the shopkeeper stay in business.
Everyone in our village faced financial hardship, as there was no steady income. I started making and selling masks to support my family, which inspired other women to make masks too. It was a trying time, but we just kept pushing on.
Eventually, we were able to speak to the panchayat (village council) about taking precautions so that social meetings could be conducted safely. Rather than an entire meet-up, we got two or three women to speak among themselves after following safety protocols, like social distancing, so they could exchange information and ideas about how to keep rumors at bay. This meant we could reach more people to get correct information out.
When the COVID-19 vaccine became available, a camp was set up in our village, with doctors, city officials, and professionals from the primary health center … but no one from the area wanted to get vaccinated. The officials asked who represented JEEViKA, and I told them I did. They asked me to go with them as nobody wanted to listen to them. So, I went to every house and talked with every woman, just as I did at the beginning of the pandemic, and I convinced them to get vaccinated. When I spoke, the women understood because they were all my fellow self-help group members. The team was very grateful to me.
These have been tough times, but we have met our goals. This work has given me a lot of confidence. I used to be very shy and preferred not to speak up, but now I can face people and speak boldly because the platform is so important. The work has given me an identity. People address me not as a wife or mother, but as an individual and as a member of JEEViKA. Like the women in my village, I also have big ambitions … and I’m sure with JEEViKA’s support, I will achieve my goals. Because of this work, I am confident about the future.
– Told to Thanh Tan, independent journalist, November 2021
Website | brlps.in

©Bill & Melinda Gates Foundation/Alex Garland
“This pandemic can ground us back in our humanity.”
Robin Martin (she/her) | Deputy Director of Strategy Planning and Management, Bill & Melinda Gates Foundation
Every day, I get up and say, no matter what position I’m in, how do I become a part of the change I really want to see? For me, it always comes back to how my own humanity is connected to everyone else.
I grew up in Knoxville, Tennessee, in a family of four – two boys, two girls. We were primarily raised by my mother, a single mother, who has always served as my inspiration. I was the first to attend and graduate college, so the lesson has always been clear to me: it takes just one person to create multi-generational change in our families.
During a little storm called Katrina, I was the athletic director at Dillard University. Katrina was my grounding moment. It didn’t matter what education you had or how much money you had, we were all standing in the FEMA line. I also saw the public response to Hurricane Katrina. People saw us as “others.” They called us refugees. In that moment, I began to want to understand when leadership worked – and when it didn’t really work, particularly for people of color. I decided then to go back and get a doctoral degree in educational leadership because I wanted to study the impact of leadership around community. I decided, “I really want to change the world.”
The foundation’s COVID-19 investment in historically black colleges and universities (HBCUs) has been my way of saying, “What is in my sphere of control?” In my current role, I run the day-to-day operations for the post-secondary success team. When the pandemic started, we knew it would have disproportionate impacts on students of color across the country. We knew many students didn’t have means to get back home, where family members were already disproportionately impacted by COVID-19. We knew HBCUs would be disproportionately impacted because of a lack of access to digital learning. So, I went to my director and said, “We have an opportunity to think about the impacts of COVID-19 on HBCUs and their students – and we have an opportunity to ensure that students are safe and return to school safely, so we can prevent more stop-outs and dropouts.”
A friend told me about the Just Project, which provided COVID-19 testing support for HBCUs. Because most HBCUs are sitting in and supporting communities of color, they already have a positive reputation in helping communities. I thought, this is one way the foundation can really leverage its power and dollars to be intentional around supporting communities of color.
HBCU support for public health was not a part of the foundation’s core strategy or things we work on in the day-to-day inside the post-secondary success team. This was a new effort – but it was needed.
We created a new network of support through an investment of $15 million in eight different institutions that all had the medical infrastructure to provide comprehensive testing, testing support and tracking for HBCUs. Then, those eight campuses then became hubs and spokes to support other HBCUs around the country. Now, HBCUs are building infrastructure to help communities become more vaccinated – and become more educated about health concerns and health disparities. That investment has allowed us to have a broader conversation around how to leverage HBCUs and Black and Brown knowledge to help communities of color find the help they need.
Part of my dissertation was on an African philosophy called Ubuntu. Ubuntu means, “I am because you are, you are because I am.” We’re struggling to achieve this thinking during this pandemic. But we need to see that our health is connected to everyone’s health – and not just locally, but also across the globe. 600,000 people needlessly died across our country over the last year in a country that has some of the best medical research and assets in the world. Meanwhile, there’s also a housing crisis and an economic crisis. We have chosen privileged capitalism and racism over ensuring that all people have access. At the same time, less than two percent of people on the continent of Africa have been fully vaccinated. Morally, we’ve lost our way if we think that that is okay.
If change is going to happen, we need audacious goals and efforts. We say, “I hope tomorrow will be better” – and yet that hope gives us an easy path to not actually act. If we were all taking some small action to see our own humanity and see how it is tied to other people, to see that we can take action in relation to a global community, then this world would be a better place.
– Told to Marcus Harrison Green, South Seattle Emerald, in April 2021
Website | usprogram.gatesfoundation.org

©Bill & Melinda Gates Foundation/Ilan Godfrey
“We see access to quality healthcare as something that should be available to everybody in Africa, without limitation.”
Marc Matthews (he/him), Business Development Director, Africa, LumiraDx
I work for LumiraDx, which is a point of care diagnostics company. The founders have worked to scale diagnostics and health technology businesses for more than 30 years. We manufacture and commercialize an innovative diagnostic platform that supports a broad menu of tests with lab comparable performance at the point of care. The platform also supports secure digital connectivity to the cloud, to integrate data into health management systems.
All of this means we give previously underserved patients direct access to fast, accurate test results – which then allows them to have a continuity of care that leads to better overall health outcomes.
I’m based in KwaZulu-Natal, South Africa and lead our African Organization, which has representatives in 14 African countries. Before the pandemic, our partnership with the Gates Foundation was about remodeling Primary Health Care on the African continent.
Following the onset of the COVID-19 pandemic in 2020, we pivoted to bring COVID-19 antigen testing to countries with limited testing infrastructure. A key objective from the start was to make sure that every life in Africa counted – and that we could make our COVID-19 antigen tests available to all 55 countries in the African Union.
Delivering results
Our diagnostic platform is small and portable, about 20 cm (7.88 in) by 10 cm (3.93 in), weighing just over a kilogram (2.2 lbs), with a digital interface. The testing process is incredibly easy. It utilizes a nasal swab drawn from the nasal cavity, rather than the less comfortable and difficult-to-reach rear of the nasopharyngeal cavity. The test reading process happens in under 12 minutes, usually while the patient waits, with results appearing right on the screen. The data is aggregated into a central data repository that informs Ministries of Health about localized increases in infection, so they can respond accordingly.
The process is simple and effective and has facilitated the rapid deployment of COVID-19 testing in a variety care settings, such as field clinics, airports, primary healthcare facilities, occupational health settings, and walk-through clinics. This has helped to strengthen access to care and allowed broader epidemiological control of the pandemic in countries that lack integration across different levels of the health system.
It is revolutionary to have instrument-based testing with lab comparable results available in community care settings. As we’ve seen, testing continues to be important because of the number of variants circulating globally, and because of low vaccination rates in parts of the world, especially in Africa – not due to a lack of need or interest, but due to a lack of infrastructure. In addition, testing is a core component of any antiviral treatment program, and COVID-specific antiviral treatments are becoming available.
Beyond the scope of the COVID-19 pandemic, our platform can also test for other diseases. We are developing tests for cardiovascular disease, diabetes, coagulation disorders and infectious diseases including tuberculosis (TB). This molecular test will enable point-of-care TB testing and increase the ability of healthcare providers in Africa to initiate earlier treatment.
Seeing the inequitable access to diagnosis and management of high-burden diseases in Africa motivates me to improve access to our technology and thereby improve health outcomes. It’s a privilege to drive change.
A more equitable future
Over the course of this pandemic, we’ve learned that we need stronger primary care systems, and that decentralizing care into outlying areas is going to allow us to adapt and respond more effectively to the next pandemic.
We’ve also learned a new way of doing business while maintaining a high level of engagement as business and health leaders. We’ve had a number of roundtable meetings among Africa’s health leaders, with strong leadership and support from the Africa CDC, and the Africa Medical Supplies Platform (AMSP), which is a single-source platform that has expedited market access. On top of that, individual countries are learning how to work more effectively to rally a response to a pandemic situation.
All of this cooperation represents a huge shift in the way things are done. It’s one positive change that has been brought about by this difficult time. There’s a resiliency, adaptability, and agility that is being created through this process – an acknowledgement for the need for preparedness going forward.
We now know that it’s possible for us to deal with this level of change – and that lesson cannot be underestimated. All of these lessons bode well for the future of healthcare worldwide.
When we talk about universal health coverage and health system strengthening, these may be big terms and big programs, but underpinning that whole process is equitable access to technology. Our team sees access to quality healthcare as a human right, as something that should be available to everybody in Africa, without limitation.
Through our partnership with the foundation, we’ve had the privilege to make that a reality. It’s important to remember that if we don’t stem the tide on COVID-19 infections, we will have continued challenges that have a major impact on global economies. It’s a reminder that what happens in Africa affects the rest of the world.
– Told to Thanh Tan, independent journalist, November 2021
Website | lumiradx.com/us-en

Photographer: David Acolatse, copyright Build Health International, location: Monrovia, Liberia
“It is supposed to be equal. Each and every person is supposed to have oxygen.”
Steve Mtewa (he/him), Biomedical and Facilities Engineer, Build Health International
I work at Build Health International. Our organization designs, builds, and raises hospital standards in rural areas and low-resource settings. We improve upon all aspects of a hospital’s physical set-up, including building construction, solar grids and electricity infrastructure, plumbing and water sanitation, and even facility maintenance.
I’ve worked in the Bahamas, Haiti, Ethiopia, Sierra Leone, Liberia, Nigeria, and Malawi – my home. And I may soon go to Madagascar.
Every site that I visit has different needs, and my work can involve a variety of tasks. It’s funny, you can tell what I’m working on at a specific location because of the nickname they give me. When I was in the Bahamas, I was “the equipment man,” because I was responsible for assessing, replacing, installing, and readying their medical equipment, such as autoclaves. In Sierra Leone, they called me “the teacher,” because I was training teams on each piece of equipment.
I got into this work years ago when I became critically ill myself. I went to visit my mom, thinking I would have to say goodbye. She was working in an extremely rural area of Malawi. The American doctors there needed someone to help with translation. They ended up admitting me to the hospital so I could help, but it also meant I was able to get further treatment. I started to get better. As I recovered, I would walk around the hospital and see these American clinicians battling with equipment that was new to them. I would help them figure out the problem. The more this continued, the more I started looking for challenges. Eventually, we had improved the hospital systems so much that this became my job and I went on to complete additional training and education.
Medical equipment works as part of the entire hospital infrastructure. Some items run on electrical circuits; others need access to running water. With everything, you need someone who understands them. I took some courses at first, but mostly I learned by doing. I was even able to build a team. I’m very proud of that team to this day.
Then, when I joined Build Health International, the first two years of my time were spent in intensive trainings. My job now is to make sure I know the system. I have someone on-site who understands the specifics of the facility and I walk them through the set-up, make sure it’s working properly, and get them trained so they can train others.
The oxygen man
As soon as COVID started, my focus became almost entirely about oxygen.
Hospitals have always needed oxygen. They need oxygen in the same way they need toilets or an incinerator. Oxygen is used during operations and as a life-saving intervention if, for example, you have a newborn who is failing to breathe or when people are struggling during a severe episode of malaria.
In less developed countries, many people die because of a lack of oxygen. Now, after COVID, the eyes of the world are opened to this problem. And, unfortunately, the oxygen needs outside of COVID have not gone away. COVID made the oxygen shortage far worse.
Treating COVID requires what we call a “high-flow” of oxygen, which refers to the liters of oxygen per minute that you give to a patient. 5 to 10 liters per minute is typical for most health needs, but with COVID it’s at least 20 or 30 liters per minute, sometimes more. Sourcing high-flow oxygen in low-resource settings can become much more difficult. We need to ensure that the equipment is calibrated correctly, because it’s like a drug. Delivering too much or too little can have consequences. It’s also like a drug in the sense that it has to be prescribed, just like painkillers or antibiotics, because oxygen is expensive to generate.
All oxygen delivery systems are not the same, and equipment from different manufacturers work differently. Oxygen comes in big heavy tanks, which can be a problem in developing countries. You can also generate oxygen with an industrial machine called a pressure swing adsorption plant, or oxygen plant, but many sites don’t have technicians with the skills to maintain and repair the plant if it breaks.
Since the pandemic, we have been visiting a variety of hospitals and doing assessments of their oxygen situation. Each country has a different challenge, but the underlying problems are common across the board … things like unreliable electricity to power oxygen systems, difficulty in transporting oxygen, steep costs, and a lack of the skills and tools necessary for local technicians to maintain systems.
That’s where we come in. When oxygen plants break, we get them working properly – then we give their on-the-ground team as much training as we can, making sure they know how to do the repairs and where to get spare parts. In many cases, we have the smaller spare parts with us, enough to cover maybe two or three repairs. For a period of time, we make our team available, so if they have a problem they can call … but the staff builds their own relationship with their machine. Over time, they learn how to make it sustainable for themselves.
Closing the gaps
Every Breath Counts is an initiative that brings together technicians, doctors, policy makers, and manufacturers. We compare problems and come up with solutions. We try to solve problems a little bit at a time because often, when we get hung up in bureaucracy, the person who suffers most is the patient. Often, it’s not because there is no oxygen, but rather because it’s expensive, or the roads are bad, making the transport of liquid oxygen dangerous, or the hospital cannot manage to renovate, or maybe the authorities believe oxygen is not their priority. It’s our job to raise concern about all of these issues before it is too late.
If COVID continues to hit Africa the way it has been, a lot of people are going to lose their lives, because – even now – the chance of a patient getting oxygen is very small.
If you visit a public hospital in some countries, I promise you will cry. You’ll see this is not how it’s supposed to be. Then, if you go to an expensive private hospital, you find that they have people with their cylinders next to them and they have a backup plan if this tank ends. But it is supposed to be equal. Each and every person is supposed to have oxygen.
This is the gap that we started trying to close with Build Health International. It’s going to take ages for this gap to fully close … but, when I see some change, it motivates me.
I’m happy that I’m one of the pioneers in this work. And I am hopeful that this pandemic has been a wake-up call to the world. Even in developed countries, oxygen is a challenge, and people die because they can’t access oxygen. This is something we’ve been saying for years doing this work, and people haven’t understood. Perhaps now they can.
– Told to Thanh Tan, independent journalist, December 2021
Website | buildhealthinternational.org

©Bill & Melinda Gates Foundation/Charina Pitzel
“I hope future generations live in a world with better public health infrastructure.”
Jordan Tappero (he, him), Deputy Director, Neglected Tropical Diseases, Global Health, Bill & Melinda Gates Foundation
I joined the Bill & Melinda Gates Foundation in 2018, working with neglected tropical diseases. That means parasites, viruses, and bacteria, categorized according to the populations that are affected by them – roughly two billion people who live in the greatest level of poverty on the planet.
As a medical epidemiologist, I had 25 years of experience with epidemics around the world before joining the foundation. I started in the Epidemic Intelligence Service (EIS) at the U.S. Centers for Disease Control and Prevention (CDC). After two years as an EIS officer, I opened CDC’s new country office in Botswana. At that time, in the mid-1990s, Botswana had the highest HIV prevalence in the world: about 38% of the population between ages 15 and 49 was HIV-infected. Simultaneously, there was a tuberculosis epidemic in sub-Saharan Africa, and the co-epidemic with HIV made for very severe tuberculosis. Later, I was the CDC Country Director in Thailand when SARS (severe acute respiratory virus) first hit in 2003. Thereafter in 2006, I was the CDC Country Director in Uganda which experienced both Marburg and Ebola outbreaks – both hemorrhagic fever viruses.
Knowing how serious respiratory virus pandemics can be, many of us in global health went into high-anxiety mode when we saw a new respiratory virus emerge in late 2019.
I had been part of an ad hoc pandemic preparedness group at the foundation with Scott Dowell and others. In early January 2020, we had confirmation that the new virus was a coronavirus, which would later be named SARS-CoV-2. Because of our knowledge and experience with SARS, we knew this new virus was going to be serious … but we didn’t know if it would be regional to Southeast Asia or a global outbreak. We weren’t using the word “pandemic” in those early days. But it was clear by the end of January that we had a pandemic.
New systems for a new threat
At that time, I was deployed to Geneva, Switzerland, to help establish a global surveillance system for COVID with the World Health Organization’s (WHO) Health Emergencies Program. The surveillance system brings together daily data collected by Ministries of Health and routes it through WHO regional offices and onwards to WHO headquarters. That’s the that you can look at online to see daily counts for global cases and deaths.
When the WHO Director-General declared the pandemic, we didn’t know if it would be possible to use contact tracing and isolation to stop ongoing spread, as we did with SARS in 2003-2004. We quickly learned that about 30-40% of all new infections were being transmitted by people who had no symptoms. That changed the calculus of our ability to stop transmission through contact tracing and isolation alone. By March or April 2020, it became clear that we were going to be less fortunate than we were with the first SARS.
When I returned to Washington state, I started working with the epidemiology and modeling team at the foundation. We used the most recent data modeling to answer questions like, “How fast is the virus spreading? How well do mitigation measures, like border closures, masks and being six feet apart, work?”
In December 2020, we saw that a new variant of concern (VOC) – which would later be called the Alpha VOC – emerged in the U.K. There wasn’t guidance from the WHO on how to do surveillance for variants, so I was sent back to Geneva in early 2021 to again work for several months with WHO’s Health Emergencies Program. My job was to set up new surveillance guidelines for variants, focusing on low- and middle-income countries so we could get more representation of possible variants emerging in those countries. Thereafter, we watched the Delta variant spread from Southeast Asia in March and April to become the predominant strain around the world, until Omicron replaced it in late 2021.
It’s clear now, after nearly two years, that we will continue to see new variants emerge. But hopefully the surveillance system we put in place will help identify new strains more quickly. Early detection gives industry a longer lead time to tweak existing tools that diagnose, prevent, and/or treat infections – or to build better tools, which we hope will be universal for any emerging variants.
It’s an honor to be able to work at the foundation and to have incredible resources and the ability to move quickly.
Health disparities – and distrust
Inequity on the surveillance question is very compelling. When we look at the global data, the vast majority of COVID cases among healthcare workers are disproportionately more women than men. I think that’s because there are more women on the front lines – who provide direct patient care as a physician or nurse. Whatever the reasons are, it’s important that vaccines become available and globally prioritized for healthcare workers and others on the front lines.
We also know that the amount of vaccine for low- and middle-income countries is a fraction compared to what high-income countries have had/acquired. The foundation anticipated this problem since the beginning of the pandemic and has been a strong voice for the equitable distribution of vaccines. For example, Gavi’s COVAX Advanced Market Commitment helps buy vaccines for low-income countries. Ensuring global access to vaccines is important because global immunity will help to prevent the emergence of new variants. What kind of a world will we have if variants are allowed to emerge unchecked? How will our vaccines work against those variants? How will the variety of other vaccines around the world work against new variants?
We’re all in this together, globally.
But this also touches closer to home. My father-in-law sadly acquired COVID just before the Holiday Season in 2020. I got to see, through his experience, how challenged our medical care system is. I had to advocate for monoclonal antibody therapeutics because his doctors weren’t aware they were available and being recommended by NIH and the CDC. Newly emerging therapies that are recommended are not always accessible because of high variability across our public and private health care system. It’s getting better … but I don’t know how people who don’t have a medical background are able to quickly access the latest therapies without some level of awareness and advocacy.
There are other challenges too. There’s so much misinformation and a general distrust about science-based sources of information. That’s a challenge perhaps even greater than SARS-CoV-2 itself. We need to educate people about the safety of these vaccines and the importance of getting vaccinated.
Hope for more equitable systems
The biggest challenge is trying to imagine a response to the questions everyone has. “When will this pandemic be over?” or “what is the world going to look like?” I don’t think anyone knows. I also don’t think there are many people who believe we can get back to a world where COVID-19 is not present in our lives for many years to come. We may not be able to say SARS-CoV-2 is gone.
My career in global public health has been highly rewarding. Through public health, we’re able to foster better lives for people now and in the future. I hope future generations live in a world with better public health systems. I hope industry has better capacity to scale up to meet emergent health threats – and that there is equitable distribution of that ability for better public health and preparedness around the world, not just in a handful of countries.
– Told to Thanh Tan, independent journalist, September 2021

©Bill & Melinda Gates Foundation/Charina Pitzel
“If we want to move out of this pandemic, the tool is vaccines.”
Vidya Sampath (she/her),
Director and Global Team
Lead for Data Analytics,
VillageReach
Erin Larsen-Cooper
(she/her), Director and
Global Team Lead for
Research, Evidence and
Learning,
VillageReach
Vidya Sampath: VillageReach is a public health and global health non-profit organization that for 20 years has focused on getting products and services, like vaccination, to people who need them. We’ve had a particular focus on vaccine delivery in sub-Saharan Africa. During the pandemic, we pivoted to apply our expertise to COVID vaccine delivery in King County and then to address vaccine inequity worldwide.
Erin Larsen-Cooper: Before COVID, it used to be difficult to describe public health, but the pandemic has helped people understand the importance of vaccine supply, logistics, and delivery. I used to think that if I wanted to go into health, I needed to be a clinician. After doing HIV-focused public health and community health work with the Peace Corps in Uganda, I got a Master’s degree in social work and public health. I’ve been at VillageReach for 10 years.
Vidya Sampath: My motivation to work in global health came from growing up in India, a country with significant disparities in finances, resources and healthcare access. From a personal standpoint, I’ve been aware of the difference it makes when you have access to healthcare. When I was quite young, my father was sick and wasn’t able to access to the services he needed – and we lost him. That experience has impacted everything that I’ve done in my life. I made my way to the U.S. for undergrad and grad school and I’ve been with VillageReach for eight years now.
Erin Larsen-Cooper: As a public health expert, I’m familiar with pandemics, but I also experienced it in the same way that most people did—reading and hearing about it.
Vidya Sampath: I remember seeing news reports in January about Wuhan. The commentary seemed to be, “What’s happening in China is really unfortunate, but that will never happen here.” I was struck by that because, being in global health, you know that’s not always true, especially as public health capacity in the U.S. is—in many ways—worse than what exists in other parts of the world.
Erin Larsen-Cooper: Honestly, I felt really scared for my family. Members of my family tested positive early on, so it quickly went from being “this is something that’s distant” to “this is happening to our family.”
Vidya Sampath: I have two very young children. We were extremely worried about my older daughter because she was born premature and has had many respiratory illnesses. My family immediately went into intense lockdown: we stopped going out and we stopped letting people in. Suddenly, my husband and I were running a home daycare for our two children while we were also working full-time jobs. It wasn’t unique to us; hundreds and thousands of families had to do this, the world over.
Erin Larsen-Cooper: Sometimes, being a part of the public health response can be comforting because you see people mobilizing; but it also makes it worse. You have access to firsthand information that can escalate fears—for example, when people were saying, “This is how many ventilators we have left.”
Vidya Sampath: In December 2020, the Pfizer vaccine got approved. That same week, the Bill & Melinda Gates Foundation called the President of VillageReach and said, “Are you available to work in your backyard?” That’s when we drew upon the bi-directional learning from Africa and Asia for the work we did with King County. VillageReach’s 20 years of expertise in strengthening vaccine delivery activities helped in us being able to jump right in.
Erin Larsen-Cooper: The foundation served as that connective tissue. They went to King County and said, “What do you need? How can we help?” And King County responded, “People. We need people.”
Vidya Sampath: “We need people who already have this knowledge.” So only 10 days before Christmas, Erin and I began to work directly with King County public health. We started out as part of that surge workforce to help get the Pfizer vaccine to frontline healthcare workers and long-term care residents. Then, between December and January, we were helping King County manage logistics, planning, workforce, cold chain, and capacity-building. We worked with moderate volume clinics (which see between 100 to 500 people a day), drive-through clinics, and large hospitals which needed to push the vaccines out all the way down to each person.
At the same time, we also started to help King County plan for mass vaccination sites that averaged 2000-3000 people a day. It wasn’t easy, especially as there was no pipeline. The county didn’t know what vaccines would arrive in the following week. I give a lot of credit to King County Public Health and their fantastic data analytics team and strategy team. They were able to say, “We’re working with limited information, so what’s the problem that we can solve for today and how do we communicate that succinctly to the public? These are the constraints, but this is how we will serve you with what we have.”
Erin Larsen-Cooper: The first high-volume site was the accesso ShoWare Center, an ice hockey stadium in Kent. We had to turn it into a vaccine site, making sure everything was accessible. We made sure the patient journey didn’t involve stairs, and we extended hours into evenings and weekends. We did whatever we could do to increase access.
Vidya Sampath: We
knew there was inequity in the way
the COVID-19 vaccine rollout
happened. By May 2021, 70% of the
King County population that was
eligible was vaccinated, but when
you disaggregate that number and
look across regions and racial lines
within King County, South King
County didn’t have as high of a
vaccination rate as other more
affluent parts of the county, even
though it bore the brunt of the
COVID-19 outbreaks. African American
and Latinx populations were still
not getting vaccinated at similar
rates to white or Asian American
populations or other groups.
King County Public Health was really
focused on this piece because they
knew this would happen. One of the
things we did was to hold back
appointments and work with community
groups to make sure underserved
communities could access
appointments. There was clear
recognition that if we want people
to get vaccinated, we have to bring
the vaccines closer to the people
where they work. And we worked with
the Community Navigator program, for
example, where people can sit with
their clients and help them register
for an appointment in other
languages.
Erin Larsen-Cooper: It was great to see that community-led response. We often had 100 staff on site, many of whom were multilingual so they could jump in and help with translation. Inequities are obviously broad and structural, but these were ways to ask, in the moment, “How can we make this as accessible as possible?”
Vidya Sampath: As
of September, all racial groups have
now achieved 70% vaccination rates.
That’s fantastic!
On the flip side, our mission at
VillageReach is also to advocate for
more resources and vaccines to be
sent to places like the African
continent. Because this is a global
pandemic, we need the rest of the
world to be vaccinated at a high
rate too. Even though vaccines are
reaching many low- and middle-income
countries, the volume isn’t
anywhere close to the volume that
high-income countries purchased for
themselves. That deep inequity, as
well as the apathy in the U.S. to
vaccine versus the real desire and
need for vaccines elsewhere, has
been interesting to witness.
If we want to move out of this pandemic–if we want to have the freedom to move around and congregate, if we want to get away from masking—the tool is vaccines. The science clearly shows that, when people who are vaccinated get the infection, they carry less viral load for potentially way less time than unvaccinated people. They’re not transmitting as much infection as unvaccinated people are.
Erin Larsen-Cooper:
I have been inspired by how much
clinicians and health workers and
public health professionals have
risen to the occasion.
Vidya Sampath: Public health clearly
has the tools, the training, and the
knowledge, but it does not have the
resources or the support.
Erin Larsen-Cooper: I feel like people have been sprinting for the length of a marathon now. That becomes even more true at smaller health departments, where a handful of people are in charge of everything COVID: they’re the contact tracers, testers, vaccinators, and the people who are advising on outbreaks. Many of them have worked every weekend for months and months and months on end with no vacations—and they’re still showing up and willing to do it.
Vidya Sampath: What I’ve been inspired by has been surprising to me. Working in South King County was the first time I spent as much time in that part of King County I moved to Seattle eight years ago, but a lot of that time I spent traveling for work––which gave me joy. When COVID hit and no one could travel, I lost my sense of purpose and I felt like I was not making a difference. But South King County is so diverse in terms of racial and cultural backgrounds, social-economic backgrounds, and life experiences. Every day I was working alongside the community that came in through the doors. And many of the people who live in South King County, it turns out, come from India. I was able to start using Indian languages again that I haven’t for eight years. I got excited to be here in King County. I thought: “This is home right now”—and it’s this work gave me an opportunity to connect with where I live.
– Told to Thanh Tan, independent journalist, September 2021
Website | villagereach.org

©Bill & Melinda Gates Foundation/Ilan Godfrey
“We’re not out of the woods. This has to be a global effort.”
Dr. Solomon Zewdu (he/him), Deputy Director, Africa office, Bill & Melinda Gates Foundation
I’m in charge of the foundation’s health and nutrition portfolio across the African continent. I’m a medical doctor by training and a U.S. Air Force medical officer, where I ran a global program focused on HIV prevention and control program in Asia and Southeast Asia – an epidemic I later worked on through the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR). I’ve also worked in disaster preparedness and mitigation: I was a first responder at the Pentagon on 9/11 in 2001 and also part of the response to the Indonesian tsunami in 2004. My international health work with Johns Hopkins and the CDC brought me in Ethiopia in 2006, and in 2015 I joined the Bill & Melinda Gates Foundation to work on end-to-end solutions for health system strengthening.
Since March 2020, I have been the African continent COVID-19 coordinator, which calls upon my background in disaster preparedness, mitigation, response, surveillance and systems logistics, and systems building. My work is all about getting the necessary intelligence: finding, aggregating, correlating, synthesizing and then presenting the most pertinent information for foundation to make investment and advocacy decisions.
The way I see it, we’re all in the trenches together. We need a global movement to fight this pandemic … and we have to start listening to low- and middle-income countries – the countries we’re trying to help. No one knows better than the folks who live it 24/7.
In community health, we talk about patient-centered design; but let’s also talk about continent-centered design and country-centered design. During the pandemic, the African continent has come together at a scale I’ve never seen before. The solidarity across the African Union is massive, and the Africa CDC has been stepping up and making a real impact. But there has also been massive inequity ever since the pandemic started.
People are familiar with the different variants’ waves, but there are equally grave inequity waves too.
When the pandemic started I was in Ethiopia, we saw three waves of inequity across the continent. The first was the lack of personal protective equipment (PPE) and testing supplies, even for frontline health workers. We simply couldn’t test enough to appreciate the extent of our local disease burden. Before we got that sorted out, a second wave came, which was a lack of supplies for treatment even while having the money to pay for it, like oxygen and Dexamethasone. The amount we received never matched the need. That still wasn’t solved before the third wave hit, which was the inequity of vaccine access. We’re still waiting for vaccines. Vaccination rates of 60-70% in high-income countries are a benchmark for global progress, but it means nothing if only 4% of the African continental population has been vaccinated. “Last mile” challenges – of making sure the vaccines get to the people rather than people to the vaccines – are real. If you think about getting vaccines to central warehouses in the Democratic Republic of the Congo (DRC) – in Kinshasa, Lagos, or Addis, for example – the work is still not done. Then, you have local equity and access issues related to employers understanding someone needs to leave work to stand in line the whole day to get vaccinated, or daycare support so someone can leave their child to go get vaccinated. In many places, it’s a massive trade-off between health and livelihood. You cannot hide at home thinking about a virus that’s potentially going to kill you when you know for a fact that, if you don’t go out and earn a living, you or your loved one could die from hunger. You won’t be able to provide that livelihood, and your family will suffer. From the very beginning, people on the African continent have had a meltdown at the family level, at the community level, and at the country level balancing the need of the community to minimize the risk of covid versus the need to prevent a socioeconomic crisis.
It has to be everybody – all governments and all resources – coming together and solving for “last mile” delivery.
There are great things happening and there’s a lot of good intent and massive innovation. Think about making a vaccine in about eight months. The technology, the effort, the knowledge that went into it was amazing. But on the other side, there are a lot of undelivered promises. This doesn’t undermine the goodwill of the people working on the pandemic; it’s the implementation that’s broken. And on the African continent, COVID-19 didn’t simply replace anything. We still have the burden of tuberculosis, malaria, HIV, Ebola, et cetera to still deal with. Routine immunization, for measles as just one example, has also taken a massive hit.
I’ll say it out loud: the global machinery needs to be more receptive to the needs and voices of African countries. We can’t pass the baton and ask the African continent to fend for itself. To get control over the pandemic, this has to be a joint global effort. COVID-19 is going to be with us for a very long time. You don’t eliminate this disease, you have to manage it – we all know that now. There will be other variants. Viruses don’t wait months or years to mutate; they can mutate at any time, which could compromise the gains we’ve had so far. We’re not out of the woods. And, with globalization, we’re all just one flight away. If COVID is anywhere, COVID is everywhere, which means we still have to deliver on the promises that have been made because it’s just a matter of time before there will be another pandemic. Not if, when.
At the same time, the African continent and Asia and Southeast Asia have been asking for decision-making rights, saying “Don’t just decide for us. Let us be part of the decision making. Make sure that we are at the table when a decision is made for us. We appreciate the goodwill and every penny, every effort, and every partnership; but we need to come together to better understand what the world should look like with COVID-19 added to it.”
That’s the insight that my
colleagues in the Africa offices and
my position contribute to the
foundation’s appreciation of
context.
It has been an amazing learning
opportunity to be a part of this
pandemic response effort and to work
with great people, but there’s
no resting yet, with the massive
amount of populations across the
entire globe not yet vaccinated and
still getting exposed at a high
rate; I realize everybody’s
tired, including myself. The scale
and timeline at which you respond is
extremely challenging on so many
levels; emotionally, intellectually,
physically. The stakes are high. The
inequity is vividly higher.
This is a life-defining moment. My nine-year-old daughter was seven when this started. She says, “Someday, I’m going to tell my grandchildren that I survived the pandemic.” As for me, I hope I don’t have any other exciting things like this for the rest of my life. I’ve had enough. But looking at the world through her eyes energizes me. Until we’re done, we’re not done.
– Told to Thanh Tan, independent journalist, September 2021